Rationale and Objectives
To compare resident workload from Emergency Department (ED) studies before and after the implementation of a required 1-hour report turnaround time (TAT) and to assess resident and faculty perception of TAT on resident education.
Materials and Methods
Resident study volume will be compared for 3 years before and 1 year after the implementation of a required 1-hour TAT. Changes to resident workload will be compared among the different radiology divisions (body, muscuolskeletal (MSK), chest, and neuro), as well as during different shifts (daytime and overnight). Residents and faculty at two Midwest institutions, both of which have a required report TAT, will be invited to participate in an online survey to query the perceived effect on resident education by implementation of this requirement. A P < .05 was considered statistically significant.
Results
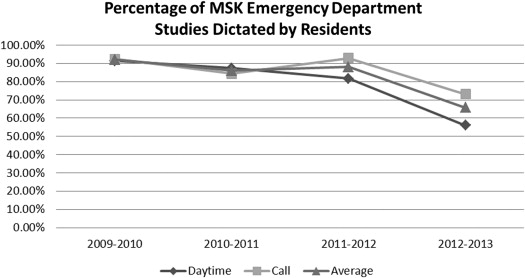
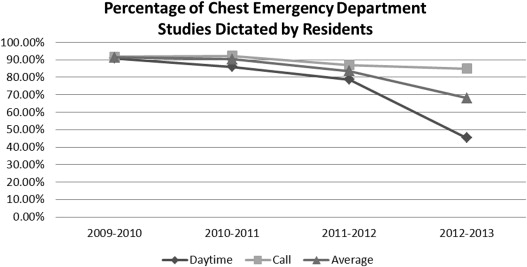
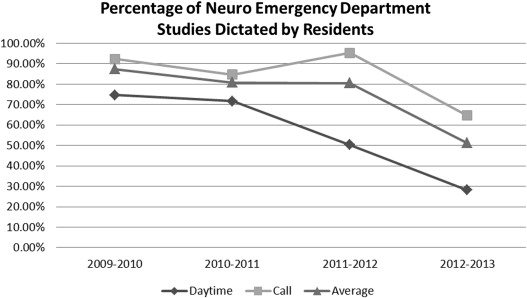
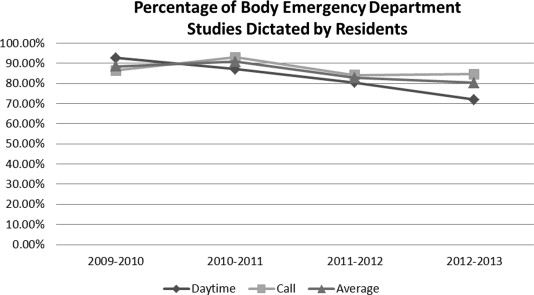
A significant decrease in resident involvement in ED studies was noted in the MSK, chest, and neuro sections with average involvement of the 3 years before the 1-hour TAT of 89%, 88%, and 82%, respectively, which decreased to 66%, 68%, and 51% after the 1-hour TAT requirement ( P < .05). The resident involvement in ED studies only mildly decreased in the body section from an average before the 1-hour TAT of 87% to 80% after the 1-hour TAT requirement ( P < .1). There was an overall significant decrease in resident ED study involvement during the daytime ( P = .01) but not after hours during resident call ( P = .1). Seventy percent of residents (43 of 61) and 55% of faculty (63 of 114) responded to our surveys. Overall, residents felt their education from ED studies during the daytime and overnight were good. However, residents who were present both before and after the implementation of a required TAT felt their education had been significantly negatively affected. Faculty surveyed thought that the required TAT negatively affected their ability to teach and decreased the quality of resident education.
Conclusions
Residents are exposed to fewer ED studies after the implementation of a required 1-hour TAT. Overall, the current residents do not feel this decreased exposure to Emergency room studies affects their education. However, residents in training before and after this requirement feel their education has been significantly affected. Faculty perceives that the required TAT negatively affects their ability to teach, as well as the quality of resident education.
Over the past several years, radiology residents have experienced major changes to their training and certification. From the growing emphasis on diagnostic milestones for resident training to the transition from an oral board examination to a more image-rich computer-based examination, radiology resident training is in a state of rapid evolution . In addition, the transition from film with tape/digitized recordings to a picture archiving and communication system (PACS) with speech recognition has dramatically changed the way academic radiologists process and review cases with residents . More recently, the effect on radiology resident education related to 24/7/365 in-house attending coverage was investigated . Another pressure now challenges academic radiologists further with a new variable to which they must adapt: the implementation of required reduced radiology report turnaround times (RTATs), potentially taking away from time spent in instruction of residents.
RTAT has increasingly become an important metric for measuring the quality of diagnostic radiology services. With the institution of PACS and speech recognition systems, RTAT has decreased over the last decade from days to near-real time . Increasingly, teleradiology companies have emphasized decreased RTAT to hospitals as a metric for improved services to compete with local radiology groups, or even other teleradiology companies . Some academic teaching hospitals have experimented with pay-for-performance programs to decrease their RTAT . This simple metric can easily be assigned a value by hospital administration and can be used to evaluate current radiology services and compare them to competing radiology services. The increased interest in this metric by radiology departments and hospital administrators over the last several years has led to hospital radiology RTAT requirements, particularly in the cases of Emergency Department (ED) studies and “stat” interpretations.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Emergency Department Study Volume
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Surveys
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Emergency Department Study Volume
Get Radiology Tree app to read full this article<
Table 1
Percent of ED Studies Dictated by Residents During Daytime (8 am –5 pm ) Hours
Average of 3 years Before Required RTAT (%) After Implementation of Required RTAT (%)P Value Body 86.71 71.87 .05 Musculoskeletal 86.79 55.98 .009 Chest 85.16 45.35 .008 Neuro 65.55 28.10 .04 All sections 81.05 50.33 .01
ED, Emergency Department; RTAT, radiology report turnaround time.
A significant decrease of resident ED study dictations during daytime hours before and after implementation of a required 1-hour RTAT was observed.
Table 2
Percent of ED Studies Dictated by Residents While on Call (5 pm –8 am )
Average of 3 years Before Required RTAT (%) After Implementation of Required RTAT (%)P Value Body 87.73 84.59 .35 Musculoskeletal 89.92 73.09 .025 Chest 90.27 85.03 .08 Neuro 90.72 64.59 .015 All sections 89.66 76.83 .1
ED, Emergency Department; RTAT, radiology report turnaround time.
No statistically significant change ( P = .1) of resident ED study involvement during call hours before and after implementation of a required 1-hour RTAT was observed.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Surveys
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Comments
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Supplementary Data
Get Radiology Tree app to read full this article<
Appendix
Get Radiology Tree app to read full this article<
References
1. http://acgme.org/acgmeweb/Portals/0/PDFs/Milestones/DiagnosticRadiologyMilestones.pdf accessed on 3/9/2015.
2. http://www.theabr.org/ic-dr-certifying-exam accessed on 3/9/2015.
3. Mullins M., Mehta A., Patel H., et. al.: Impact of PACS on the education of radiology residents: the residents’ perspective. Acad Radiol 2001; 8: pp. 67-73.
4. Collins J., Gruppen L., Bailey J., et. al.: 24/7/365 in-house radiologist coverage: effect on resident education. Acad Radiol 2014; 21: pp. 842-850.
5. Mattern C., King B., Hangiandreou , et. al.: Electronic imaging impact on image and report turnaround times. Journal of Digital Imaging 1999; 12: pp. 155-159.
6. White K.: Speech recognition implementation in radiology. Pediatr Radiol 2005; 35: pp. 841-846.
7. Bhan , Coblentz C., Norman G., et. al.: Effect of voice recognition on radiologist reporting time. CARJ 2008; 59: pp. 203-209.
8. Hawk P.: Teleradiology: friend or foe? What imaging’s now indispensable partner means for radiology’s future and for the quality of care. J Health Care Finance 2011; 37: pp. 71-92.
9. Boland G., Halpern E., Gazelle G.S.: Radiologist report turnaround time: impact of pay-for-performance measures. AJR 2010; 195: pp. 707-711.
10. Lowe R., Abbuhl S., Baumritter A., et. al.: Radiology services in emergency medicine residency programs: a national survey. Acad Emerg Med 2002; 9: pp. 587-594.
11. Joffe S., Burak J., Rackson M., et. al.: The effect of international teleradiology attending radiologist coverage on radiology residents’ perception of night call. J Am Coll 2006; 3: pp. 872-878.
12. Branstetter B., Morgan M., Nesbit C., et. al.: Preliminary reports in the emergency department: is a subspecialist radiologist more accurate than a radiology resident?. Acad Radiol 2007; 14: pp. 201-206.
13. Dell C, Deloney L, Hicks B, Jambhekar K. Preserving the educational value of call in a diagnostic radiology residency program. January 2014. J Am Coll Radiol; 11:68–73.
14. Ruchman R.B., Jaeger J., Wiggins E.F., et. al.: Preliminary radiology resident interpretations versus final attending radiologist interpretations and the impact on patient care in a community hospital. AJR Am J Roentgenol 2007; 180: pp. 523-526.
15. Velmahos G.C., Fili C., Vassiliu P., et. al.: Around-the-clock attending radiology coverage is essential to avoid mistakes in the care of trauma patients. Am Surg 2001; 67: pp. 1175-1177.
16. Cohen M.D., Gunderman R.B., Frank M.S., et. al.: Challenges facing radiology educators. J Am Coll Radiol 2005; 2: pp. 681-687.
17. Lundmerer K.M.: Instilling professionalism in medical education. JAMA 1999; 282: pp. 881-882.
18. Collins J.: Keys to educator effectiveness in radiology. Acad Radiol 2006; 13: pp. 641-643.
19. Huang B.K., Lubner M., Resnik C.: Balancing clinical service and education in the radiology residency. Acad Radiol 2009; 16: pp. 1161-1165.
20. DeFlorio R., Coughlin B., Coughlin R., et. al.: Process modification and emergency department radiology service. Emerg Radiol 2008; 15: pp. 408-412.