Rationale and Objectives
This study sought to more definitely illustrate the impact and feasibility of implementing a low-dose protocol for computed tomography (CT)-guided biopsies using size-specific dose estimates and multivariate analyses.
Materials and Methods
Fifty consecutive CT-guided lung and extrapulmonary biopsies were reviewed before and after implementation of a low-dose protocol (200 patients total, mean age 61 ± 15 years, 128 women). Analyses of variance with Bonferroni correction were used to compare standard and low-dose protocols in terms of patient demographics, physician experience, target lesion size, total dose-length product, total acquisitions, size-specific dose estimate, signal-to-noise ratio, contrast-to-noise ratio, and lesion conspicuity ratings. All procedures were performed on the same 16-slice CT scanner.
Results
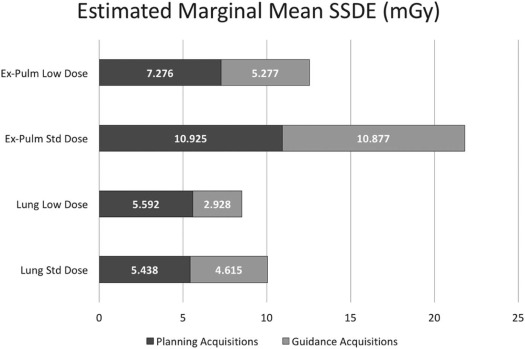
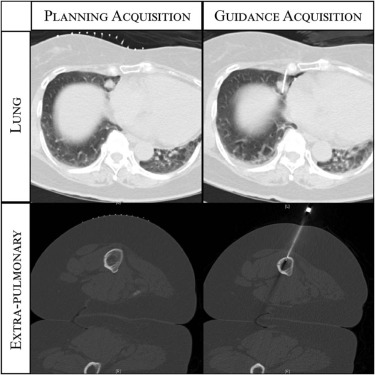
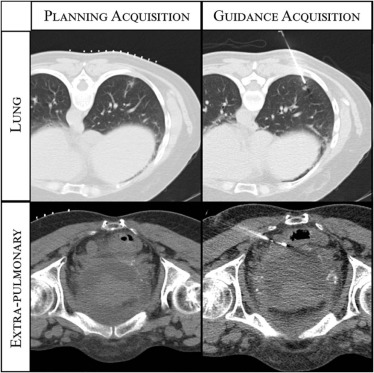
Voluntary protocol adherence was 100% (lung) and 89% (extrapulmonary). The low-dose protocol achieved significantly lower total average dose-length product [(lung) 735.6 ± 599.4 mGy × cm to 252.1 ± 101.9 mGy × cm, P < .001; (extrapulmonary) 724.7 ± 545.0 mGy × cm to 392.9 ± 239.5 mGy × cm, P < .001] and size-specific dose estimate [(lung) 5.2 ± 0.8 mGy × cm to 4.3 ± 1.5 mGy, P < .001; (extrapulmonary) 10.1 ± 6.7 mGy to 6.5 ± 2.7 mGy, P < .001]. Only the change in protocol was independently associated with lower size-specific dose estimates when controlling for the other variables ( P < .0001). This was achieved with no significant differences in signal-to-noise ratio, contrast-to-noise ratio, or lesion conspicuity.
Conclusions
Implementation of a low-dose protocol for CT-guided biopsies resulted in 21% and 36% of size-specific dose estimate reduction for lung and extrapulmonary biopsies, respectively, with excellent adherence. Interventional and body radiologists should implement low dose CT-guidance protocols aiming to improve patient safety.
Introduction
Despite the many benefits of computed tomography (CT), its widespread use over the last several decades has dramatically increased patients’ average radiation exposure from medical imaging. Data supporting a cause-and-effect relationship are limited, but there is a general consensus that carcinogenesis is a stochastic effect of ionizing radiation, with a linear risk-dose relationship. As such, in 2007, it was estimated that 29,000 future cancers and 14,500 deaths would be related to CT scans performed in the United States .
Dose reduction has been an important focus in diagnostic radiology but less so for CT-guided procedures as adequate guidance can be prioritized over dose reduction efforts. Adoption of diagnostic appropriateness criteria and use of lower tube energies and iterative reconstruction techniques can each reduce dose while achieving similar image quality . Previous studies suggest similar techniques can significantly reduce radiation exposure during CT-guided biopsies, but most of these investigations did not control for important confounders or adjust dose parameters for patient size, limiting the strength of their findings.
Get Radiology Tree app to read full this article<
Materials and Methods
CT Guidance Protocols
Get Radiology Tree app to read full this article<
Table 1
CT Guidance Protocol Parameters
Protocol Acquisition Type Scan Type kVp mA mAs CTDI vol Gantry Rotation Pitch Collimation Low-dose lung protocol Planning Helical 120 120 60 4.2 0.5 0.8 1.5 Guiding Sequential 100 100 50 2.25 0.5 1 1.5 Standard lung protocol Planning Helical 120 120 60 4.2 0.5 0.8 1.5 Guiding Helical 120 120 60 4.2 0.5 0.8 1.5 Low-dose ex-pulm protocol Planning Helical 120 120 80 5.6 0.5 0.8 1.5 Guiding Sequential 100 100 80 3.6 0.5 1 1.5 Standard ex-pulm protocol Planning Helical 120 120 80 5.6 0.5 0.8 1.5 Guiding Helical 120 120 80 5.6 0.5 0.8 1.5
CT, computed tomography; CTDIvol, computed tomography dose index volume (mGy); ex-pulm, extrapulmonary; kVp, kilovolt potential peak; mA, milliamperes; mAs, milliampere seconds.
Gantry rotation time expressed in seconds, pitch expressed as a ratio of the table feed to the detector width, and collimation expressed in millimeters.
Get Radiology Tree app to read full this article<
Biopsy Cohorts and Technique
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Data Collection
Get Radiology Tree app to read full this article<
SSDE=a×e−b×AP×LAT√×CTDIvol SSDE
=
a
×
e
−
b
×
A
P
×
L
A
T
×
C
T
D
I
v
o
l
where a = 3.70 and b = 0.0367 are previously defined constants ; AP and LAT are in cm; and SSDE is in mGy. Lesion density, density standard deviation, and the attenuation of the adjacent parenchyma were measured for lung biopsies to calculate contrast-to-noise ratio (CNR) and signal-to-noise ratio (SNR) values according to the technique by Heyer et al. :
CNR=(DensityLesion−DensityLung Parenchyma)/Standard DeviationLesion CNR
=
(
Density
Lesion
−
Density
Lung Parenchyma
)
/
Standard Deviation
Lesion
SNR=DensityLesion/Standard DeviationLesion SNR
=
Density
Lesion
/
Standard Deviation
Lesion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Data Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Lung Biopsy Statistics
Parameter Standard-dose Protocol (n = 50) Low-dose Protocol (n = 50)P Value Gender (M/F) 14/36 17/33 .52 Age (y) 65 ± 15 67 ± 13 .43 Lesion size (cm) 2.0 ± 1.6 2.1 ± 1.2 .97 Physician (T/A) 40/10 36/14 .35 Total DLP (mGy × cm) 735.6 ± 599.4 252.1 ± 101.9 <.001 Total acquisitions 17 ± 8 15 ± 6 .13 Planning SSDE (mGy) 5.6 ± 0.8 5.6 ± 0.9 .99 Guidance SSDE (mGy) 4.7 ± 0.7 3.0 ± 0.4 <.001
DLP, dose-length product; M/F, male/female; SSDE, size-specific dose estimate; T/A, trainee/attending.
Data reported as mean ± standard deviation unless indicated otherwise. P values are for univariate comparisons.
Table 3
Extrapulmonary Biopsy Statistics
Parameter Standard-dose Protocol (n = 50) Low-dose Protocol (n = 50)P Value Gender (M/F) 16/34 25/25 .07 Age (y) 56 ± 16 57 ± 16 .84 Physician (T/A) 39/11 33/17 .19 Total DLP (mGy × cm) 724.7 ± 545.0 392.9 ± 239.5 <.001 Total acquisitions 13 ± 6 14 ± 7 .48 Planning SSDE (mGy) 10.1 ± 6.7 7.7 ± 2.9 .02 Guidance SSDE (mGy) 10.1 ± 6.7 5.2 ± 1.7 <.001
DLP, dose-length product; M/F, male/female; SSDE, size-specific dose estimate; T/A, trainee/attending.
Data reported as mean ± standard deviation unless indicated otherwise. P values are for univariate comparisons.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
SNR:−0.5±7.1(standard dose)vs0.2±3.0(low dose),P=.52 SNR
:
−
0.5
±
7.1
(
standard dose
)
vs
0.2
±
3.0
(
low dose
)
,
P
=
.52
CNR:33.7±19.5(standard dose)vs33.3±26.2(low dose),P=.93 CNR
:
33.7
±
19.5
(
standard dose
)
vs
33.3
±
26.2
(
low dose
)
,
P
=
.93
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
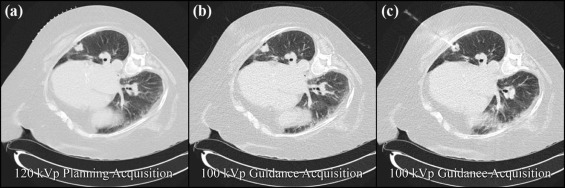
SNR:0.2±3.0(120kVp)vs0.3±2.8(100kVp),P=.43 SNR
:
0.2
±
3.0
(
120
kVp
)
vs
0.3
±
2.8
(
100
kVp
)
,
P
=
.43
CNR:33.3±26.2(120kVp)vs25.8±18.9(100kVp),P=.11 CNR
:
33.3
±
26.2
(
120
kVp
)
vs
25.8
±
18.9
(
100
kVp
)
,
P
=
.11
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Berrington de Gonzalez A., Mahesh M., Kim K.P., et. al.: Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med 2009; 169: pp. 2071-2077.
2. Leipsic J., Labounty T.M., Heilbron B., et. al.: Estimated radiation dose reduction using adaptive statistical iterative reconstruction in coronary CT angiography: the ERASIR study. AJR Am J Roentgenol 2010; 195: pp. 655-660.
3. Lu G.M., Luo S., Meinel F.G., et. al.: High-pitch computed tomography pulmonary angiography with iterative reconstruction at 80 kVp and 20 mL contrast agent volume. Eur Radiol 2014; 24: pp. 3260-3268.
4. Willemink M.J., Leiner T., de Jong P.A., et. al.: Iterative reconstruction techniques for computed tomography part 2: initial results in dose reduction and image quality. Eur Radiol 2013; 23: pp. 1632-1642.
5. Adiga S., Athreya S.: Safety, efficacy, and feasibility of an ultra-low dose radiation protocol for CT-guided percutaneous needle biopsy of pulmonary lesions: initial experience. Clin Radiol 2014; 69: pp. 709-714.
6. Frisch B.K., Slebocki K., Mammadov K., et. al.: Implementation of ultra-low-dose lung protocols in CT-guided lung biopsies: feasibility and safety in the clinical setting. J Int Med Res 2017; 45: pp. 2101-2109.
7. Kallianos K.G., Elicker B.M., Henry T.S., et. al.: Instituting a low-dose CT-guided lung biopsy protocol. Acad Radiol 2016; 23: pp. 1130-1136.
8. Meng X.X., Kuai X.P., Dong W.H., et. al.: Comparison of lung lesion biopsies between low-dose CT-guided and conventional CT-guided techniques. Acta Radiol 2013; 54: pp. 909-915.
9. Motamedi K., Levine B.D., Seeger L.L., et. al.: Success rates for computed tomography-guided musculoskeletal biopsies performed using a low-dose technique. Skeletal Radiol 2014; 43: pp. 1599-1603.
10. Smith J.C., Jin D.H., Watkins G.E., et. al.: Ultra-low-dose protocol for CT-guided lung biopsies. J Vasc Interv Radiol 2011; 22: pp. 431-436.
11. Tam A.L., Ensor J.E., Zvavanjanja R.C., et. al.: JOURNAL CLUB: standardizing CT-guided biopsy procedures: patient dose and image noise. AJR Am J Roentgenol 2015; 205: pp. W390-W399.
12. National Lung Screening Trial Research Team, Aberle D.R., Adams A.M., et. al.: Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365: pp. 395-409.
13. Christner J.A., Braun N.N., Jacobsen M.C., et. al.: Size-specific dose estimates for adult patients at CT of the torso. Radiology 2012; 265: pp. 841-847.
14. Ruiz-Santana S., Arboleda Sanchez J.A., Abiles J., et. al.: [Guidelines for specialized nutritional and metabolic support in the critically-ill patient. Update. Consensus of the Spanish Society of Intensive Care Medicine and Coronary Units-Spanish Society of Parenteral and Enteral Nutrition (SEMICYUC-SENPE): nutritional assessment]. Med Intensiva 2011; 35: pp. 12-16.
15. Heyer C.M., Mohr P.S., Lemburg S.P., et. al.: Image quality and radiation exposure at pulmonary CT angiography with 100- or 120-kVp protocol: prospective randomized study1. Radiology 2007; 245: pp. 577-583.
16. Gupta S., Wallace M.J., Cardella J.F., et. al.: Quality improvement guidelines for percutaneous needle biopsy. J Vasc Interv Radiol 2010; 21: pp. 969-975.
17. Bhatia R.S., Dudzinski D.M., Milford C.E., et. al.: Educational intervention to reduce inappropriate transthoracic echocardiograms: the need for sustained intervention. Echocardiography 2014; 31: pp. 916-923.