Rationale and Objectives
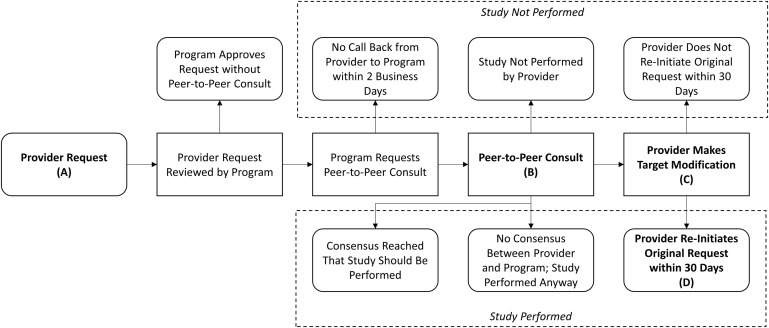
This study explored four common sequences of interaction between providers and a collaborative, nondenial model preauthorization program to assess the extent to which the collaborative consultation impacted care delivered to a patient in the 30 days after a neuroimaging consult. In each of the sequences examined, providers interacted with the preauthorization program’s consulting radiologist and modified their imaging study requests during the interaction. If providers did not subsequently reinitiate the original study requests, then it suggests that the study resulting from the collaborative consultation fulfilled the providers’ clinical objective.
Materials and Methods
Four years of retrospective authorization and clinical data were analyzed to determine the rate at which requests modified through peer-to-peer consultation were reinitiated in the following four sequences: 1) request for head computed tomography (CT) modified to head magnetic resonance imaging (MRI), 2) request for both head CT and intracranial CT angiography (CTA) or both head MRI and intracranial MRA modified to a request for a single study, 3) request for both a CT of the head and sinuses modified to a request for a single study, and 4) request for an MRI of the head and orbits modified to a request for a single study.
Results
In three of the sequences, no provider reinitiated a study within 30 days. In the fourth sequence, only 4 of 64 (6%) withdrawn requests for head CT/MRI or head CTA/MRA were reinitiated within 30 days.
Conclusions
Modifications after collaborative consultations rarely lead to repeat imaging requests, confirming the utility of the consultations.
Rationale and objectives
Although dramatic annual increases in spending on medical imaging have recently abated , there continues to be excessive imaging utilization . Unnecessary imaging can cause inconvenience to the patient, add to the cost of health care, and/or expose the patient to unnecessary ionizing radiation. Several measures have been taken to curb unnecessary utilization, including installing physician order entry decision support systems at sites of care, reducing reimbursements for imaging studies through the Deficit Reduction Act of 2005 and requiring clinicians to have their plans reviewed by preauthorization services , There has been some evidence that other factors such as preauthorization may have played a role in the recent slowdown, as the reduction in utilization has been greater in hospitals, where the reimbursement reduction from the Deficit Reduction Act of 2005 did not apply . Research on the impact of consultative preauthorization on practice patterns has been limited, and given the multitude of initiatives to decrease utilization, a drop in utilization is not an inherent indicator of the success of consultative preauthorization. Although it has been shown in aggregate that providers within a single radiology department are unlikely to reinitiate computed tomography (CT) and magnetic resonance imaging (MRI) studies after interacting with a consultative preauthorization process, little attention has been paid to the impact of preauthorization on utilization in specific clinical sequences .
One concern has been that preauthorization needlessly encumbers physicians by requiring them to engage in extra steps that may not improve the quality of care . Preauthorization services work to modify the studies that providers order when the studies are not warranted by evidence-based guidelines. Although these modifications may improve the quality of care delivered, quality could suffer if preauthorization suggestions do not meet provider needs. One indicator of whether preauthorization recommendations do not meet provider needs is the extent to which providers reinitiate study requests that had previously been modified by the preauthorization process. When this occurs, patients may be inconvenienced by having to receive imaging over multiple sessions, instead of in one session. The objective of this study was to evaluate the extent to which clinical consultations related to neuroimaging requests meet clinical objectives by examining the frequency with which providers reinitiate study requests.
Preauthorization Process
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Data Source and Sample Population
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Outcomes
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Preauthorization Program Interaction Sequences
Sequence Neuroimaging Request Collaborative Consult Action Target Modification Action Indicating Reinitiation of Original Request 1 Head CT Provider requests head CT, but the consulting radiologist recommends a head MRI. Head CT modified to head MRI and approved Provider reinitiates head CT request 2 Head CT/MRI + head CTA/MRA Provider requests both head CT and intracranial CTA or both head MRI and intracranial MRA, but the consulting radiologist recommends withdrawal of one of the requests. One study approved, other study withdrawn Provider reinitiates request for withdrawn study 3 Head CT + sinus/skullbase CT Provider requests both a CT of the head and sinuses. The consulting radiologist recommends just a head CT unless sinus disease is highly suspected. One study approved, other study withdrawn Provider reinitiates request for withdrawn study 4 Head MRI + orbital MRI Provider requests an MRI of the head and orbits. The consulting radiologist recommends scanning the area where they suspect the problem is located before proceeding with the second. One study approved, other study withdrawn Provider reinitiates request for withdrawn study
CT, computed tomography; CTA, computed tomography angiography; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 2
Results
Sequence Instances with Neuroimaging Request (n) Instances with Collaborative Consults (n) Requests Modified, n (% ∗ ) Reinitiation of Original Request Within 30 Days n % † (95% CI) Head CT to head MRI 6454 993 411 (41.4) 0 0.0 (0.0–0.9) head CT/MRI + head CTA/MRA (1 withdrawn) 1103 164 64 (39.0) 4 6.3 (1.7–15.2) Head CT + sinus/skullbase CT (1 withdrawn) 113 64 19 (29.7) 0 0.0 (0.0–17.6) Head MRI + orbital MRI (1 withdrawn) 20 12 8 (66.7) 0 0.0 (0.0–36.9) Total 7690 1233 502 (40.7) 4 0.8 (0.2–2.0)
CT, computed tomography; CTA, computed tomography angiography; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Limitations
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Lee D.W., Duszak R., Hughes D.R.: Comparative analysis of Medicare spending for medical imaging: sustained dramatic slowdown compared with other services. American Journal of Roentgenology 2013; 201: pp. 1277-1282.
2. Levin D.C., Rao V.M., Parker L.: JACR 2012; 9: pp. 795-798.
3. Alliance W.H.Choosing wisely in Washington State.2014.Washington Health AllianceSeattle, Washington:
4. Department of Health and Human Services: Medicare Program; Revisions to Payment Policies Under the Physician Fee Schedule for Calendar Year 2006 and Certain Provisions Related to the Competitive Acquisition Program of Outpatient Drugs and Biologicals Under Part B. Federal Register 2005; 70: pp. 70116-70476.
5. Yousem D.M.: Combating overutilization: radiology benefits managers versus order entry decision support. Neuroimaging Clin N Am 2012; 22: pp. 497-509.
6. Levin D.C., Rao V.M., Parker L.: Physician orders contribute to high-tech imaging showdown. Health Affairs 2010; 29: pp. 189-195.
7. Friedman D.P., Smith N.S., Bree R.L., et. al.: Experience of an academic neuroradiology division participating in a utilization management program. JACR 2009; 6: pp. 119-124.
8. McAneny B.L.: Report 5 of the Council on Medical Service (I-09): radiology benefits managers.2009.American Medical AssociationChicago, Illinois
9. Robinson J.D., Hippe D.S., Hiatt M.D.: The effect of a no-denial policy on imaging utilization. Journal of the American College of Radiology 2013; 10: pp. 501-506.
10. Friedman D.P., Smith N.S.: Variability in study withdrawal rates among academic neuroradiologists participating in a radiology utilization management program. JACR 2011; 8: pp. 716-719.
11. Levin D.C., Bree R.L., Rao V.M., et. al.: A pre-authorization program of a radiology benefits management company and how it has affected utilization of advanced diagnostic imaging. Journal of the American College of Radiology : JACR 2010; 7: pp. 33-38.
12. Mitchell J.M., LaGalia R.R.: Controlling the escalating use of advanced imaging: the role of radiology benefit management programs. Medical Care Research and Review 2009; 66: pp. 339-351.
13. Duszak R., Berlin J.W.: Utilization management in radiology, part 1: rationale, history, and current status. JACR 2012; 9: pp. 694-699.