Rationale and Objectives
Lymphoscintigraphy may be used for diagnosing secondary lymphedema. Dermal backflow, the presence of radiotracer in dermal lymphatics, is a key clinical feature. Although often reported as present or absent, a scale that assesses the severity of dermal backflow has been previously developed. The aim of this study was to determine the reliability of these two methods of assessment.
Materials and Methods
Sixteen experienced nuclear medicine physicians assessed the quantity of dermal backflow of 57 lymphoscintigraphy scans using a 4-point descriptive scale that was dichotomized for secondary analysis. Each scan included images from four time points for women previously diagnosed with secondary lymphedema ( n = 47) and controls ( n = 5); five scans were presented twice to examine intraobserver reliability. This was further investigated as 13 physicians viewed the scans again on an Apple iPad2. The physicians rated their confidence in their scoring. Readers were blinded to clinical history.
Results
Although both the 2- and 4-point scale had moderate interobserver reliability, the reliability of the 2-point scale was slightly higher (4-point: Fleiss κ = .418, standard error [SE] = .008); 2-point: Fleiss κ = .574, SE = .013). Low interobserver reliability was found when only control subjects were considered (Fleiss κ = 0.055, SE = 0.034). Intraobserver reliability of the five repeated images varied from poor to perfect (Cohen κ = .063 to 1.00), whereas moderate to substantial intraobserver reliability (Cohen’s κ = .342 to .752) was found when comparing devices. The readers were highly confident of their scores.
Conclusions
Overall, moderate intraobserver and interobserver reliability was found for quantifying dermal backflow with both the 2- and 4-point scale.
Lymphoscintigraphy is a relatively noninvasive nuclear medicine technique used to investigate the function and anatomy of the lymphatic system . It is commonly conducted for sentinel node determination in the assessment of breast cancer or melanoma . It also can be used to assess the function and drainage patterns of peripheral lymphatics, aiding in the diagnosis and assessment of lymphatic disorders . In the setting of lymphedema secondary to treatment for breast cancer, lymphoscintigraphy has traditionally been considered the “gold standard” for confirmation of the clinical diagnosis and has been used to predict the improvement from decongestive physical therapy , to stage the severity of the lymphedema , or to assist with decisions regarding surgical intervention .
Lymphoscintigraphy involves the injection of a radiotracer subcutaneously or subdermally into the affected and unaffected limbs. Typically with upper limb lymphedema, the radiotracer is injected into the webspaces of the hand, after which both upper limbs are assessed . While both quantitative and qualitative appraisals can be completed with lymphoscintigraphy imaging, the qualitative assessment of the morphologic features seen on the lymphoscintigraphic image is more frequently considered in a clinical situation . A number of key features are reported in the qualitative assessment, including the presence of lymph nodes, the symmetry of the lymphatic pathways, and the presence or absence of dermal backflow .
Get Radiology Tree app to read full this article<
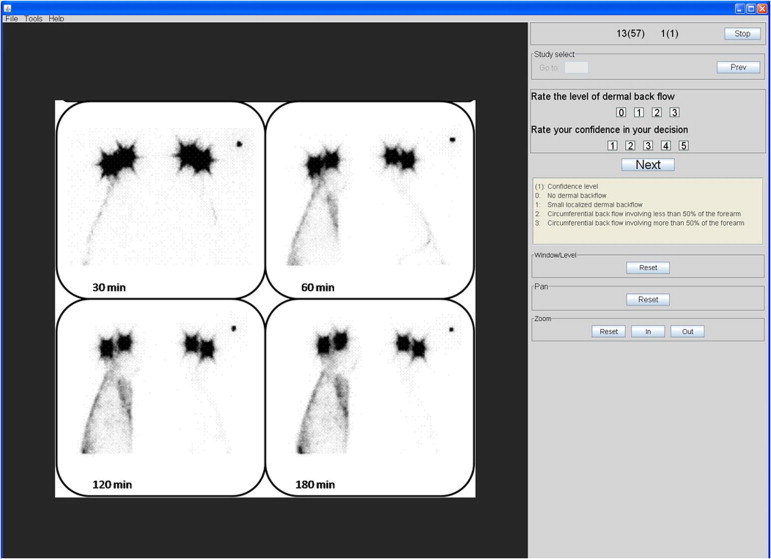
Figure 1
Example of a delayed image demonstrating dermal backflow in right hand and forearm of a woman with lymphedema secondary to treatment for breast cancer. Image was taken 180 minutes post injection of the radioisotope 99m Tc-antimony colloid.
Get Radiology Tree app to read full this article<
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Data analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Nuclear Medicine Physicians Characteristics
Readers ( N = 16) Age (y) ∗ 54.4 (9.0) Sex (M:F) 13:3 Cases/week viewed ∗ 161.9 (128.5) Experience in nuclear medicine (y) ∗ 21.7 (10.8)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 2
Variability of Scoring Recorded for a Single Scan
No. of Scoring Options Selected by Readers No. of Scans ∗ (%) 1 1 (2) 2 19 (33) 3 20 (35) 4 17 (30)
Get Radiology Tree app to read full this article<
Table 3
Number of Readers Who Scored the Control Scans as Normal (No Dermal Backflow Present)
Control Subject No, of Readers ∗ (Range of Scores Given) Control Images That Were Repeated 1 13 (0 to 2) 2 6 (0 to 2) 5 (0 to 3) 3 11 (0 to1) 4 8 (0 to 3) 7 (0 to 3) 5 12 (0 to 3)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Bourgeois P., Leduc O., Belgrado J.P., et. al.: Scintigraphic investigations of the superficial lymphatic system: quantitative differences between intradermal and subcutaneous injections. Nucl Med Commun 2009; 30: pp. 270-274.
2. Lyman G.H., Giuliano A.E., Somerfield M.R., et. al.: American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol 2005; 23: pp. 7703-7720.
3. Uren R.F., Howman-Giles R., Chung D., et. al.: Guidelines for Lymphoscintigraphy and F18 FDG PET Scans in Melanoma. J Surg Oncol 2011; 104: pp. 405-419.
4. Szuba A., Shin W.S., Strauss H.W., et. al.: The third circulation: Radionuclide lymphoscintigraphy in the evaluation of lymphedema. J Nucl Med 2003; 44: pp. 43-57.
5. Szuba A., Strauss W., Sirsikar S.P., et. al.: Quantitative radionuclide lymphoscintigraphy predicts outcome of manual lymphatic therapy in breast cancer-related lymphedema of the upper extremity. Nucl Med Commun 2002; 23: pp. 1171-1175.
6. Gebousky P., Karny M., Krizova H., et. al.: Staging of upper limb lymphedema from routine lymphoscintigraphic examinations. Comput Bio Med 2009; 39: pp. 1-7.
7. Lee B.B., Bergan J.J.: New clinical and laboratory staging systems to improve management of chronic lymphedema. Lymphology 2005; 38: pp. 122-129.
8. Scarsbrook A.F., Ganeshan A., Bradley K.M.: Pearls and pitfalls of radionuclide imaging of the lymphatic system. Part 2: evaluation of extremity lymphoedema. Br J Radiol 2007; 80: pp. 219-226.
9. Tartaglione G., Rubello D.: The evolving methodology to perform limb lymphoscintigraphy: From rest to exercise acquisition protocol. Microvasc Res 2010; 80: pp. 540-544.
10. Sty J.R., Boedecker R.A., Scanlon G.T., et. al.: Radionuclide dermal backflow in lymphatic obstruction. J Nucl Med 1979; 20: pp. 905-906.
11. Yamamoto T., Yamamoto N., Doi K., et. al.: Indocyanine Green-Enhanced Lymphography for Upper Extremity Lymphedema: A Novel Severity Staging System Using Dermal Backflow Patterns. Plast Reconstr Surg 2011; 128: pp. 941-947.
12. Yamamoto T., Matsuda N., Doi K., et. al.: The Earliest Finding of Indocyanine Green Lymphography in Asymptomatic Limbs of Lower Extremity Lymphedema Patients Secondary to Cancer Treatment: The Modified Dermal Backflow Stage and Concept of Subclinical Lymphedema. Plast Reconstr Surg 2011; 128: pp. 314E-321E.
13. Brennan P.C., McEntee M., Evanoff M., et. al.: Ambient Lighting: Effect of Illumination on Soft-Copy Viewing of Radiographs of the Wrist. AJR Am J Roentgenol 2007; 188: pp. W177-W180.
14. Brennan P.C., Ryan J., Evanoff M., et. al.: The Impact of Acoustic Noise Found Within Clinical Departments on Radiology Performance. Acad Radiol 2008; 15: pp. 472-476.
15. Wade C., Brennan P.C.: Assessment of monitor conditions for the display of radiological diagnostic images and ambient lighting. Br J Radiol 2004; 77: pp. 465-471.
16. Tsopelas C.: Particle size analysis of 99m Tc-labeled and unlabeled antimony trisulfide and rhenium sulfide colloids intended for lymphoscintigraphic application. J Nucl Med 2001; 42: pp. 460-466.
17. Borjesson S., Hakansson M., Bath M., et. al.: A software tool for increased efficiency in observer performance studies in radiology. Radiat Protect Dosimetry 2005; 114: pp. 45-52.
18. Fleiss J.L., Cohen J.: Equvalence of weighted kappa and intraclass correlation coefficient as measures of reliability. Educ Psychol Measure 1973; 33: pp. 613-619.
19. Cohen J.: A coefficient of agreement for nominal scales. Educ Psychol Measure 1960; 20: pp. 37-46.
20. Sim J., Wright C.C.: The kappa statistic in reliability studies: Use, interpretation, and sample size requirements. Physl Ther 2005; 85: pp. 257-268.
21. Chang A. Cohen’s and Fleiss’s Kappa program Concordance in ordinal data. 2011 [cited 2012 16/10/2012]; Available from: http://www.stattools.net/CohenKappa_Pgm.php .
22. Keeley V.: The use of lymphoscintigraphy in the management of chronic oedema. J Lymphoedema 2006; 1: pp. 42-57.
23. Buck A.K., Herrmann K., Stargardt T., et. al.: Economic evaluation of PET and PET/CT in oncology: evidence and methodologic approaches. J Nucl Med 2010; 51: pp. 401-412.
24. Weissleder H., Weissleder R.: Lymphedema- evaluation of qualitative and quantitative lymphoscintigraphy in 238 patients. Radiology 1988; 167: pp. 729-735.
25. Robinson P.J.: Radiology’s Achilles’ heel: error and variation in the interpretation of the Rontgen image. Br J Radiol 1997; 70: pp. 1085-1098.
26. Pinto A., Brunese L.: Spectrum of diagnostic errors in radiology. World J Radiol 2010; 2: pp. 377-383.
27. Moran M., Ryan J., Higgins M., et. al.: Poor agreement between operators on grading of the placenta. J Obstet Gynaecol 2011; 31: pp. 24-28.
28. Nelitz M., Guenther K.P., Gunkel S., et. al.: Reliability of radiological measurements in the assessment of hip dysplasia in adults. Br J Radiol 1999; 72: pp. 331-334.
29. Bellamy N., Klestov A., Muirden K., et. al.: Perceptual variation in categorizing individuals according to American College of Rheumatology classification criteria for hand, knee, and hip osteoarthritis (OA): observations based on an Australian Twin Registry study of OA. J Rheumatol 1999; 26: pp. 2654-2658.
30. Buijze G.A., Guitton T.G., van Dijk C.N., et. al.: Training Improves Interobserver Reliability for the Diagnosis of Scaphoid Fracture Displacement. Clin Orthop Relat Res 2012; 470: pp. 2029-2034.
31. Ward L.C.: Is BIS Ready for Prime Time As The Gold Standard. J Lymphoedema 2009; 4: pp. 52-56.