Rationale and Objectives
Our research team has developed a magnetic resonance imaging (MRI)-compatible robot for long bone biopsy. The robot is intended to enable a new workflow for bone biopsy in pediatrics under MRI imaging. Our long-term objectives are to minimize trauma and eliminate radiation exposure when diagnosing children with bone cancers and bone infections. This article presents our robotic systems, phantom accuracy studies, and workflow analysis.
Materials and Methods
This section describes several aspects of our work including the envisioned clinical workflow, the MRI-compatible robot, and the experimental setup. The workflow consists of five steps and is intended to enable the entire procedure to be completed in the MRI suite. The MRI-compatible robot is MR Safe, has 3 degrees of freedom, and a remote center of motion mechanism for orienting a needle guide. The accuracy study was done in a Siemens Aera 1.5T scanner with a long bone phantom. Four targeting holes were drilled in the phantom.
Results
Each target was approached twice at slightly oblique angles using the robot needle guide for a total of eight attempts. A workflow analysis showed the average time for each targeting attempt was 32 minutes, including robot setup time. The average 3D targeting error was 1.39 mm with a standard deviation of 0.40 mm. All of the targets were successfully reached.
Conclusion
The results showed the ability of the robotic system in assisting the radiologist to precisely target a bone phantom in the MRI environment. The robot system has several potential advantages for clinical application, including the ability to work at the MRI isocenter and serve as a steady and precise guide.
Introduction
This paper describes our work in developing a magnetic resonance imaging (MRI)-compatible robot for long bone biopsy in pediatrics. The robot is intended to enable a novel clinical workflow for image-guided bone biopsy with the goals of minimizing trauma and eliminating radiation exposure in children with bone cancers and bone infections.
Bone pain is a common complaint in children. It can be caused by benign etiologies such as bone infection or malignant etiologies such as bone tumor. Typically, pediatric patients present with symptoms including pain, tenderness, or reluctance to bear weight or use the affected limb. Fevers can be seen in patients with both infections and cancers. Conventional radiographs may be normal, especially early in the course of a disease. MRI is often used to aid in the diagnosis due to its improved soft tissue, marrow, and joint space resolution. The MRI appearance of infectious and neoplastic bone pathology can overlap and sometimes may be indistinguishable. However, clinical management and treatment of these etiologies is quite different.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Related Work
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Categories of Related MRI-compatible Robots
Category Type Subcategory References Clinical application Needle-based procedures Rehabilitation Mounting method Patient-mounted Bed-mounted Actuation method Pneumatic/hydraulic Piezoelectric motor MR classification: ASTM F2503 MR Conditional MR Safe
ASTM, American Society for Testing and Materials; MR, magnetic resonance; MRI, magnetic resonance imaging.
Get Radiology Tree app to read full this article<
Clinical Application
Get Radiology Tree app to read full this article<
Mounting Method
Get Radiology Tree app to read full this article<
Actuation Method
Get Radiology Tree app to read full this article<
MR Classification
Get Radiology Tree app to read full this article<
Materials and Methods
Get Radiology Tree app to read full this article<
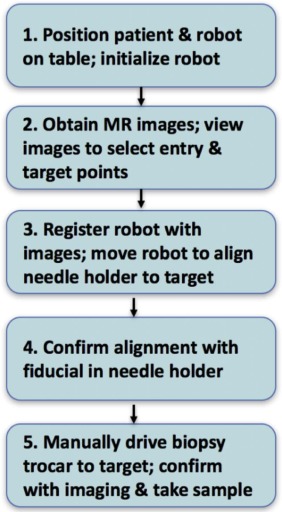
Clinical Workflow
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
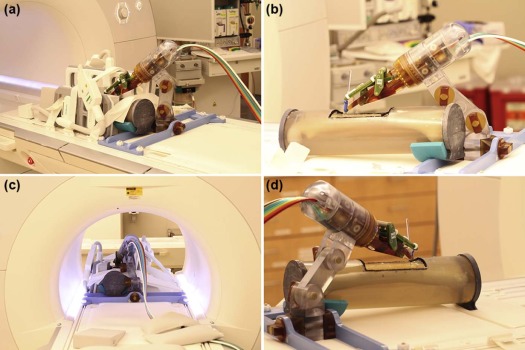
MRI-compatible Robot
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
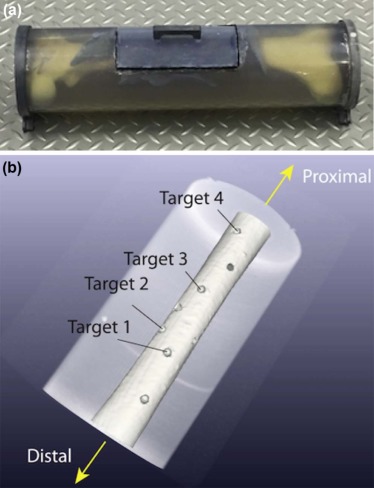
Experimental Setup: Targeting Accuracy
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
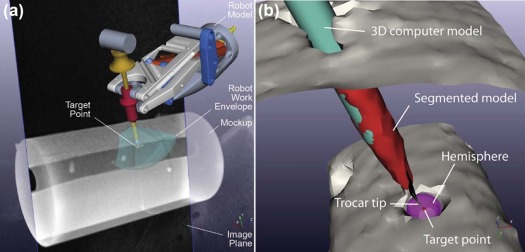
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Workflow Results
Get Radiology Tree app to read full this article<
Table 2
Time Required for Each Targeting Attempt (All Numbers in Minutes, First Four Rows Are Estimates, Last Five Rows Are From DICOM Time Stamps)
Experiment 1 2 Average Standard Deviation Test 1 2 3 4 1 2 3 4 Robot and mockup mounting on MR table (approx.) 5 5 5 0 Robot cable connection and robot homing (approx.) 6 6 6 0 Robot positioning with RCM at skin entry point (approx.) 5 5 5 0 MR coil placement (approx.) 3 3 3 0 MRI scan for registration 3.78 3.78 2.27 2.27 3.80 3.78 3.78 3.78 3.41 0.70 Image-robot registration 3.05 3.25 3.50 3.38 3.77 3.52 3.35 3.57 3.42 0.22 Robotic orientation of needle guide on target and setting the depth of needle insertion 0.72 1.13 0.65 0.80 0.65 0.87 1.17 1.00 0.87 0.21 Manual needle insertion (approx.) 2.50 2.50 2.50 2.50 2.50 2.50 2.50 2.50 2.50 0 MRI scan for targeting error measurement 2.85 2.77 2.28 2.30 3.78 3.78 3.78 3.78 3.17 0.67 Total time 31.90 32.43 30.20 30.25 33.50 33.45 33.58 33.63 32.37 1.46
MR, magnetic resonance; MRI, magnetic resonance imaging, RCM, remote center of motion.
Get Radiology Tree app to read full this article<
Targeting Experiment Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Results From Eight Targeting Trials
Target Trial Target Depth (mm) Needle Insertion Angle (Deg) 2D Error (mm)] 3D Error (mm) Medial-lateral Superior-inferior 1 1 27.34 18.86 −11.22 1.17 1.25 2 21.69 28.60 2.74 0.67 0.69 2 1 30.14 −6.52 16.97 1.50 1.68 2 26.23 −7.06 −6.55 1.31 1.51 3 1 26.74 18.92 −10.43 1.35 1.35 2 22.20 −10.10 7.72 0.69 1.01 4 1 28.02 6.72 2.88 1.58 1.71 2 26.29 −4.40 9.81 1.72 1.89 Max 1.72 1.89 Average (accuracy) 1.25 1.39 SD (precision) 0.39 0.40
SD, standard deviation.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Gutierrez K.: Bone and joint infections in children. Pediatr Clin North Am 2005; 52: pp. 779-794.
2. Dartnell J., Ramachandran M., Katchburian M.: Haematogenous acute and subacute paediatric osteomyelitis: a systematic review of the literature. J Bone Joint Surg Br 2012; 94: pp. 584-595.
3. Vasudevan V., Cheung M.C., Yang R., et. al.: Pediatric solid tumors and second malignancies: characteristics and survival outcomes. J Surg Res 2010; 160: pp. 184-189.
4. National Cancer Institute : Cancer in children and adolescents. National Cancer Institute. [Online]; Available at: https://www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
5. Siddiqui M.M., Rais-Bahrami S., Turkbey B., et. al.: Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 2015; 313: pp. 390-397.
6. Tsekos N.V., Khanicheh A., Christoforou E., et. al.: Magnetic resonance-compatible robotic and mechatronics systems for image-guided interventions and rehabilitation: a review study. Annu Rev Biomed Eng 2007; 9: pp. 351-387.
7. Gassert R., Burdet E., Chinzei K.: Opportunities and challenges in MR-compatible robotics. IEEE Eng Med Biol Mag 2008; 27: pp. 15-22.
8. Moreira P., Van De Steeg G., Krabben T., et. al.: The MIRIAM Robot: a novel robotic system for MR-guided needle insertion in the prostate. J Med Robot Res 2016; pp. 1750006.
9. Stoianovici D., Kim C., Srimathveeravalli G., et. al.: MRI-safe robot for endorectal prostate biopsy. IEEE ASME Trans Mechatron 2014; 19: pp. 1289-1299.
10. Stoianovici D., Kim C., Petrisor D., et. al.: MR Safe robot, FDA clearance, safety and feasibility prostate biopsy clinical trial. IEEE ASME Trans Mechatron 2016; 22: pp. 115-126.
11. Estévez N., Yu N., Brügger M., et. al.: A reliability study on brain activation during active and passive arm movements supported by an MRI-compatible robot. Brain Topogr 2014; 27: pp. 731-746.
12. Yap H.K., Kamaldin N., Lim J.H., et. al.: A magnetic resonance compatible soft wearable robotic glove for hand rehabilitation and brain imaging. IEEE Trans Neural Syst Rehabil Eng 2016; 25: pp. 782-793.
13. Monfaredi R., Wilson E., Sze R., et. al.: Shoulder-mounted robot for MRI-guided arthrography: accuracy and mounting study.Engineering in Medicine and Biology Society (EMBC), 2015 37th annual international conference of the IEEE.2015.pp. 3643-3646.
14. Hata N., Song S.E., Olubiyi O., et. al.: Body-mounted robotic instrument guide for image-guided cryotherapy of renal cancer. Med Phys 2016; 43: pp. 843-853.
15. Melzer A., Gutmann B., Remmele T., et. al.: INNOMOTION for percutaneous image-guided interventions. IEEE Eng Med Biol Mag 2008; 27: pp. 66-73.
16. Franco E., Brujic D., Rea M., et. al.: Needle-guiding robot for laser ablation of liver tumors under MRI guidance. IEEE ASME Trans Mechatron 2016; 21: pp. 931-944.
17. Van den Bosch M.R., Moman M.R., van Vulpen M., et. al.: MRI-guided robotic system for transperineal prostate interventions: proof of principle. Phys Med Biol 2010; 55: pp. N133.
18. Su H., Shang W., Cole G., et. al.: Piezoelectrically actuated robotic system for MRI-guided prostate percutaneous therapy. IEEE ASME Trans Mechatron 2015; 20: pp. 1920-1932.
19. Stoianovici D., Patriciu A., Petrisor D., et. al.: A new type of motor: pneumatic step motor. IEEE ASME Trans Mechatron 2007; 12: pp. 98-106.
20. Stoianovici D., Jun C., Lim S., et. al.: Multi-Imager Compatible, MR Safe, Remote Center of Motion Needle-Guide Robot. IEEE Trans Biomed Eng 2017; PP(99):1-1
21. Chen Y., Kwok K.-W., Tse Z.T.H.: An MR-conditional high-torque pneumatic stepper motor for MRI-guided and robot-assisted intervention. Ann Biomed Eng 2014; 42: pp. 1823-1833.
22. Price K.D., Sin V.W., Mougenot C., et. al.: Design and validation of an MR-conditional robot for transcranial focused ultrasound surgery in infants. Med Phys 2016; 43: pp. 4983-4995.
23. Schouten M.G., Ansems J., Renema W., et. al.: The accuracy and safety aspects of a novel robotic needle guide manipulator to perform transrectal prostate biopsies. Med Phys 2010; 37: pp. 4744-4750.
24. Stoianovici D., Whitcomb L.L., Anderson J.H., et. al.: A modular surgical robotic system for image guided percutaneous procedures.International Conference on Medical Image Computing and Computer-Assisted Intervention.1998.SpringerBerlin:pp. 404-410.
25. Stoianovici D., Cleary K., Patriciu A., et. al.: AcuBot: a robot for radiological interventions. IEEE Trans Robot Autom 2003; 19: pp. 927-930.
26. Lorensen W.E., Cline H.E.: Marching cubes: a high resolution 3D surface construction algorithm.1987.pp. 163-169.
27. Besl P.J., McKay N.D.: A method for registration of 3-D shapes. IEEE Trans Pattern Anal Mach Intell 1992; 14: pp. 239-256.
28. Pearson K.: LIII. On lines and planes of closest fit to systems of points in space. Lond Edinb Dublin Philos Mag J Sci 1901; 2: pp. 559-572.
29. Barile A., Arrigoni F., Zugaro L., et. al.: Minimally invasive treatments of painful bone lesions: state of the art. Med Oncol 2017; 34: pp. 53.
30. Sciulli R.L., Daffner R.H., Altman D.T., et. al.: CT-guided iliosacral screw placement: technique and clinical experience. AJR Am J Roentgenol 2007; 188: pp. W181-W192.
31. Blake-Toker A.-M., Hawkins L., Nadalo L., et. al.: CT guided percutaneous fixation of sacroiliac fractures in trauma patients. J Trauma Acute Care Surg 2001; 51: pp. 1117-1121.
32. Routt M.C., Nork S.E., Mills W.J.: Percutaneous fixation of pelvic ring disruptions. Clin Orthop 2000; 375: pp. 15-29.