Rationale and Objectives
We aimed to investigate the relationship between shear wave speed (SWS) of the lesion on preoperative breast ultrasonography (US) and disease-free survival of patients with primary operable invasive breast cancer.
Materials and Methods
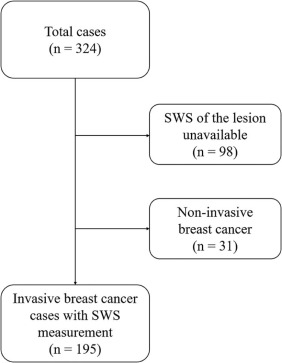
This retrospective study was approved by our Institutional Review Board. The requirement for informed consent was waived. A total of 195 consecutive newly diagnosed invasive breast cancer patients (age 33–83 years; mean 54.0 years) with preoperative breast US with SWS measurement of the lesion were identified. They underwent surgery between May 2012 and May 2013. SWS was measured at the center and three marginal zones in the main tumors, and the maximum value was used for analyses. For 35 patients who underwent primary systemic therapy (PST), the maximum SWS before PST was used. Cox proportional hazards modeling was used to identify the relationship between clinical-pathologic factors and disease-free survival.
Results
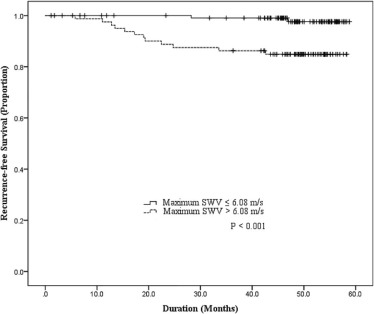
Fourteen recurrences occurred at 6–47 months (mean 22.3 months) after surgery. On multivariate analysis, a positive history of PST (hazard ratio [HR] = 4.93; 95% confidence interval [CI]: 1.66, 14.70; P = .004), adjuvant chemotherapy (HR = 3.67; 95% CI: 1.11, 12.1; P = .033), and higher maximum SWS (HR = 1.55; 95% CI: 1.07, 2.23; P = .020) were associated with poorer disease-free survival.
Conclusion
Higher maximum SWS on preoperative US, in addition to a positive history of PST and adjuvant chemotherapy, was significantly associated with poorer disease-free survival of patients with invasive breast cancer.
Introduction
Breast cancer is one of the most common malignancies and a leading cause of cancer mortality among women. Although a multidisciplinary approach including the development of screening and adjuvant therapy has improved the mortality rate , there are still more than 500,000 women who die from this malignancy per year worldwide . In planning therapeutic options for each breast cancer patient, it is beneficial to develop a prognosis. Studies have shown that information acquired from preoperative images including breast magnetic resonance imaging (MRI) can be used as prognostic factors .
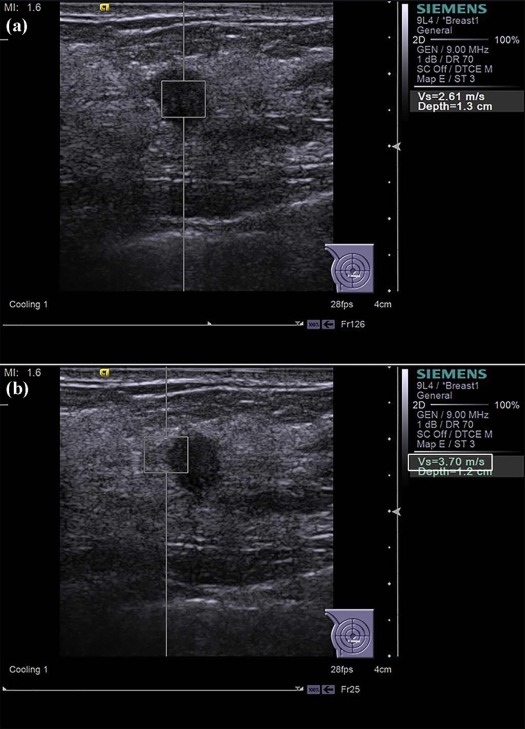
Shear wave elastography is a method of quantitatively measuring tissue elasticity during breast ultrasonography (US) examinations. Focused acoustic radiation force pushing pulses of short duration and the speed of the shear waves that are propagated in a direction orthogonal to the direction of the tissue are measured . The shear wave speed (SWS) of the lesion reflects tissue stiffness. SWS can easily be measured in clinical settings, and its use has been reported to improve accuracy in differentiating breast cancers and benign lesions when used in addition to B-mode ultrasound during breast screening and diagnosis. In addition, several studies have shown that shear wave elastography of breast cancer lesions is significantly associated with prognostic factors, including tumor size, immunohistochemical biomarkers, lymph node metastasis, and vascular and lymphovascular invasion . From these results, it is plausible that shear wave elastography could be useful for predicting outcomes, including tumor recurrence and metastasis, although these correlations have not been evaluated in previous investigations.
Get Radiology Tree app to read full this article<
Materials and Methods
Study Population
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Preoperative US Examinations
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Clinical-Pathologic Evaluation
Get Radiology Tree app to read full this article<
Statistical Analyses
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Study Subjects
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Characteristics of the Study Subjects According to Recurrence Status
Total
( N = 195) Nonrecurrence Group
( n = 181) Recurrence Group
( n = 14)P Age (y) \* 33–83 (54.0) 33–83 (54.3) 34–82 (49.4) .078 Lesion size (mm) \* 4–53 (19.0) 4–53 (18.3) 11–42 (27.4) .001 Maximum SWS (m/s) \* 2.07–8.38 (5.39) 2.07–8.38 (5.29) 4.38–8.24 (6.71) .005 Lymphadenopathy .10 Positive 37 32 5 Negative 158 149 9 Nuclear grade .098 1 or 2 169 (86.7) 159 (81.5) 10 (5.1) 3 26 (13.3) 22 (11.3) 4 (2.1) ER status .045 Positive 165 (84.6) 156 (80.0) 9 (4.6) Negative 30 (15.4) 25 (12.8) 5 (2.6) PgR status .011 Positive 144 (73.8) 138 (70.8) 6 (3.1) Negative 51 (26.2) 43 (22.1) 8 (4.1) HER2 overexpression .021 Positive 25 (12.8) 20 (10.3) 5 (2.6) Negative 170 (87.2) 161 (82.6) 9 (4.6) PST .001 Performed 35 (17.9) 27 (13.8) 8 (4.1) Not performed 160 (82.1) 154 (79.0) 6 (3.1) Type of surgery .59 Lumpectomy 85 (43.6) 80 (41.0) 5 (2.6) Mastectomy 110 (56.4) 101 (51.8) 9 (4.6) Adjuvant chemotherapy .001 Performed 59 (30.3) 49 (25.1) 10 (5.1) Not performed 136 (69.7) 132 (67.7) 4 (2.1) Adjuvant hormone therapy .004 Performed 150 (76.9) 144 (73.8) 6 (3.1) Not performed 45 (23.1) 37 (19.0) 8 (4.1) Adjuvant radiation therapy 1.0 Performed 90 (46.2) 84 (43.1) 6 (3.1) Not performed 105 (53.8) 97 (49.7) 8 (4.1)
ER, estrogen receptor; HER2, human epidermal growth factor receptor-2; PgR, progesterone receptor; PST, primary systemic therapy; SWS, shear wave speed
Unless otherwise noted, data are numbers of patients, with percentages in parentheses.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Cox Proportional Hazard Model Analyses
Get Radiology Tree app to read full this article<
Table 2
Results of Univariate Cox Proportional Hazard Analysis
HR 95% CI_P_ Age 0.96 0.91, 1.01 .123 Maximum diameter of lesion 1.074 1.03, 1.12 .001 Maximum SWS 1.62 1.12, 2.36 .011 Lymphadenopathy 2.61 0.87, 7.78 .086 Positive compared to negative Nuclear grade 2.65 0.83, 8.45 .10 1 or 2 compared to 3 ER status 3.01 1.01, 8.99 .048 Negative compared to positive PgR status 3.68 1.28, 10.62 .016 Negative compared to positive HER2 overexpression 4.14 1.38, 12.36 .011 Positive compared to negative PST 6.80 2.36, 19.62 <.001 Performed compared to not performed Type of surgery 1.40 0.47, 4.18 .547 Lumpectomy vs mastectomy Adjuvant chemotherapy 6.22 1.95, 19.83 .002 Performed compared to not performed Adjuvant hormone therapy 5.05 1.75, 14.57 .003 Not performed compared to performed Adjuvant radiation therapy 0.83 0.29, 2.39 .73 Performed compared to not performed
CI, confidence interval; ER, estrogen receptor; HER2, human epidermal growth factor receptor-2; HR, hazard ratio; PgR, progesterone receptor; PST, primary systemic therapy; SWS, shear wave speed.
Table 3
Results of Multivariate Cox Proportional Hazard Analysis
HR 95% CI_P_ PST 4.93 1.66, 14.70 .004 Performed compared to not performed Adjuvant chemotherapy 3.67 1.11, 12.1 .033 Performed compared to not performed Maximum SWS 1.55 1.07, 2.23 .020
CI, confidence interval; HR, hazard ratio; PST, primary systemic therapy; SWS, shear wave speed.
Get Radiology Tree app to read full this article<
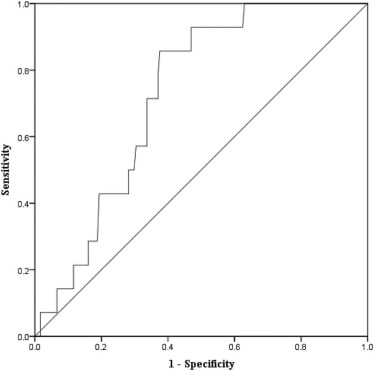
Disease-free Survival Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Berry D.A., Cronin K.A., Plevritis S.K., et. al.: Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 2005; 353: pp. 1784-1792.
2. Munoz D., Near A.M., van Ravesteyn N.T., et. al.: Effects of screening and systemic adjuvant therapy on ER-specific US breast cancer mortality. J Natl Cancer Inst 2014; 106:
3. Torre L.A., Bray F., Siegel R.L., et. al.: Global cancer statistics, 2012. CA Cancer J Clin 2015; 65: pp. 87-108.
4. Kim J.J., Kim J.Y., Kang H.J., et. al.: Computer-aided diagnosis-generated kinetic features of breast cancer at preoperative MR imaging: association with disease-free survival of patients with primary operable invasive breast cancer. Radiology 2017; 284: pp. 45-54.
5. Pickles M.D., Lowry M., Gibbs P.: Pretreatment prognostic value of dynamic contrast-enhanced magnetic resonance imaging vascular, texture, shape, and size parameters compared with traditional survival indicators obtained from locally advanced breast cancer patients. Invest Radiol 2016; 51: pp. 177-185.
6. Yi A., Cho N., Im S.A., et. al.: Survival outcomes of breast cancer patients who receive neoadjuvant chemotherapy: association with dynamic contrast-enhanced MR imaging with computer-aided evaluation. Radiology 2013; 268: pp. 662-672.
7. Li S.P., Makris A., Beresford M.J., et. al.: Use of dynamic contrast-enhanced MR imaging to predict survival in patients with primary breast cancer undergoing neoadjuvant chemotherapy. Radiology 2011; 260: pp. 68-78.
8. Shiina T., Nightingale K.R., Palmeri M.L., et. al.: WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 1: basic principles and terminology. Ultrasound Med Biol 2015; 41: pp. 1126-1147.
9. Lee E.J., Jung H.K., Ko K.H., et. al.: Diagnostic performances of shear wave elastography: which parameter to use in differential diagnosis of solid breast masses?. Eur Radiol 2013; 23: pp. 1803-1811.
10. Au F.W., Ghai S., Moshonov H., et. al.: Diagnostic performance of quantitative shear wave elastography in the evaluation of solid breast masses: determination of the most discriminatory parameter. AJR Am J Roentgenol 2014; 203: pp. W328-W336.
11. Li D.D., Xu H.X., Guo L.H., et. al.: Combination of two-dimensional shear wave elastography with ultrasound breast imaging reporting and data system in the diagnosis of breast lesions: a new method to increase the diagnostic performance. Eur Radiol 2016; 26: pp. 3290-3300.
12. Ko K.H., Jung H.K., Kim S.J., et. al.: Potential role of shear-wave ultrasound elastography for the differential diagnosis of breast non-mass lesions: preliminary report. Eur Radiol 2014; 24: pp. 305-311.
13. Choi J.S., Han B.K., Ko E.Y., et. al.: Additional diagnostic value of shear-wave elastography and color Doppler US for evaluation of breast non-mass lesions detected at B-mode US. Eur Radiol 2016; 26: pp. 3542-3549.
14. Lee S.H., Chang J.M., Kim W.H., et. al.: Added value of shear-wave elastography for evaluation of breast masses detected with screening US imaging. Radiology 2014; 273: pp. 61-69.
15. Ianculescu V., Ciolovan L.M., Dunant A., et. al.: Added value of Virtual Touch IQ shear wave elastography in the ultrasound assessment of breast lesions. Eur J Radiol 2014; 83: pp. 773-777.
16. Chang J.M., Won J.K., Lee K.B., et. al.: Comparison of shear-wave and strain ultrasound elastography in the differentiation of benign and malignant breast lesions. AJR Am J Roentgenol 2013; 201: pp. W347-W356.
17. Tozaki M., Isobe S., Fukuma E.: Preliminary study of ultrasonographic tissue quantification of the breast using the acoustic radiation force impulse (ARFI) technology. Eur J Radiol 2011; 80: pp. e182-e187.
18. Evans A., Whelehan P., Thomson K., et. al.: Invasive breast cancer: relationship between shear-wave elastographic findings and histologic prognostic factors. Radiology 2012; 263: pp. 673-677.
19. Evans A., Rauchhaus P., Whelehan P., et. al.: Does shear wave ultrasound independently predict axillary lymph node metastasis in women with invasive breast cancer?. Breast Cancer Res Treat 2014; 143: pp. 153-157.
20. Choi W.J., Kim H.H., Cha J.H., et. al.: Predicting prognostic factors of breast cancer using shear wave elastography. Ultrasound Med Biol 2014; 40: pp. 269-274.
21. Au F.W., Ghai S., Lu F.I., et. al.: Quantitative shear wave elastography: correlation with prognostic histologic features and immunohistochemical biomarkers of breast cancer. Acad Radiol 2015; 22: pp. 269-277.
22. Xie J., Wu R., Xu H.X., et. al.: Relationship between parameters from virtual touch tissue quantification (VTQ) imaging with clinicopathologic prognostic factors in women with invasive ductal breast cancer. Int J Clin Exp Pathol 2014; 7: pp. 6644-6652.
23. Zhu J., Xiong G., Trinkle C., et. al.: Integrated extracellular matrix signaling in mammary gland development and breast cancer progression. Histol Histopathol 2014; 29: pp. 1083-1092.
24. Provenzano P.P., Inman D.R., Eliceiri K.W., et. al.: Collagen density promotes mammary tumor initiation and progression. BMC Med 2008; 6: pp. 11.
25. Levental K.R., Yu H., Kass L., et. al.: Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell 2009; 139: pp. 891-906.
26. Rabasco P., Caivano R., Simeon V., et. al.: Can diffusion-weighted imaging and related apparent diffusion coefficient be a prognostic value in women with breast cancer?. Cancer Invest 2017; 35: pp. 92-99.
27. Costantini M., Belli P., Rinaldi P., et. al.: Diffusion-weighted imaging in breast cancer: relationship between apparent diffusion coefficient and tumour aggressiveness. Clin Radiol 2010; 65: pp. 1005-1012.
28. Wasif N., Garreau J., Terando A., et. al.: MRI versus ultrasonography and mammography for preoperative assessment of breast cancer. Am Surg 2009; 75: pp. 970-975.
29. Ramirez S.I., Scholle M., Buckmaster J., et. al.: Breast cancer tumor size assessment with mammography, ultrasonography, and magnetic resonance imaging at a community based multidisciplinary breast center. Am Surg 2012; 78: pp. 440-446.
30. Deurloo E.E., Tanis P.J., Gilhuijs K.G., et. al.: Reduction in the number of sentinel lymph node procedures by preoperative ultrasonography of the axilla in breast cancer. Eur J Cancer 2003; 39: pp. 1068-1073.
31. Bedrosian I., Bedi D., Kuerer H.M., et. al.: Impact of clinicopathological factors on sensitivity of axillary ultrasonography in the detection of axillary nodal metastases in patients with breast cancer. Ann Surg Oncol 2003; 10: pp. 1025-1030.
32. Cho N., Moon W.K., Han W., et. al.: Preoperative sonographic classification of axillary lymph nodes in patients with breast cancer: node-to-node correlation with surgical histology and sentinel node biopsy results. AJR Am J Roentgenol 2009; 193: pp. 1731-1737.
33. Cosgrove D.O., Berg W.A., Dore C.J., et. al.: Shear wave elastography for breast masses is highly reproducible. Eur Radiol 2012; 22: pp. 1023-1032.