Rationale and Objectives
The increasing spread of high-field and ultra-high-field magnetic resonance imaging (MRI) scanners has encouraged new discussion of the safety aspects of MRI. Few studies have been published on possible cognitive effects of MRI examinations. The aim of this study was to examine whether changes are measurable after MRI examinations at 1.5 and 7 T by means of transcranial magnetic stimulation (TMS).
Materials and Methods
TMS was performed in 12 healthy, right-handed male volunteers. First the individual motor threshold was specified, and then the cortical silent period (SP) was measured. Subsequently, the volunteers were exposed to the 1.5-T MRI scanner for 63 minutes using standard sequences. The MRI examination was immediately followed by another TMS session. Fifteen minutes later, TMS was repeated. Four weeks later, the complete setting was repeated using a 7-T scanner. Control conditions included lying in the 1.5-T scanner for 63 minutes without scanning and lying in a separate room for 63 minutes. TMS was performed in the same way in each case. For statistical analysis, Wilcoxon’s rank test was performed.
Results
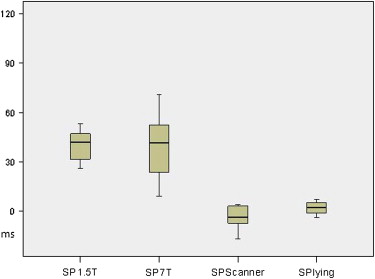
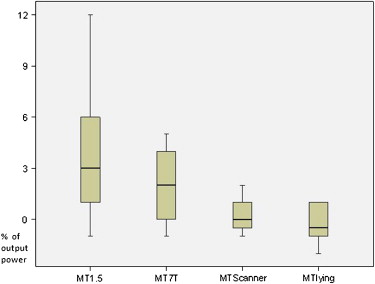
Immediately after MRI exposure, the SP was highly significantly prolonged in all 12 subjects at 1.5 and 7 T. The motor threshold was significantly increased. Fifteen minutes after the examination, the measured value tended toward normal again. Control conditions revealed no significant differences.
Conclusion
MRI examinations lead to a transient and highly significant alteration in cortical excitability. This effect does not seem to depend on the strength of the static magnetic field.
Magnetic resonance imaging (MRI) has been used in medical imaging and diagnostics for >25 years. Over this period, >300 million MRI examinations have been performed . Only a few incidents and injuries have occurred, mostly in relation to the nonobservance of common precautions and the examination of patients with implants not suitable for MRI . Generally, MRI is considered to be a harmless and safe procedure in routine clinical practice that is not associated with any ionizing radiation exposure or any permanent influence on the human body.
Higher magnetic field strengths have advantages such as higher signal-to-noise ratios and thus the possibility to achieve higher spatial resolution . This is the main reason MRI scanners with higher field strengths (>3 T) are increasingly being installed as investigational devices. The discussion of the biologic effects and the possible impact of higher magnetic fields on the human body has thus regained momentum.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Material and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
References
1. Moller H.E., von Cramon D.Y.: Bestandsaufnahme zu Risiken durch statische Magnetfelder im Zusammenhang mit der Ultrahochfeld-MRT. Rofo 2008; 180: pp. 293-301.
2. Shellock F.G., Crues J.V.: MR procedures: biologic effects, safety, and patient care. Radiology 2004; 232: pp. 635-652.
3. Kraff O., Theysohn J.M., Maderwald S., et. al.: MRI of the knee at 7.0 Tesla. Rofo 2007; 179: pp. 1231-1235.
4. Theysohn J.M., Maderwald S., Kraff O., et. al.: Subjective acceptance of 7 Tesla MRI for human imaging. MAGMA 2008; 21: pp. 63-72.
5. Lopez-Ibor J.J., Lopez-Ibor M.I., Pastrana J.I.: Transcranial magnetic stimulation. Curr Opin Psychiatry 2008; 21: pp. 640-644.
6. Kastrup O., Leonhardt G., Kurthen M., et. al.: Cortical motor reorganization following early brain damage and hemispherectomy demonstrated by transcranial magnetic stimulation. Clin Neurophysiol 2000; 111: pp. 1346-1352.
7. Rossini P.M., Barker A.T., Berardelli A., et. al.: Non-invasive electrical and magnetic stimulation of the brain, spinal cord and roots: basic principles and procedures for routine clinical application. Report of an IFCN committee. Electroencephalogr Clin Neurophysiol 1994; 91: pp. 79-92.
8. International Electrotechnical Commission: International standard, medical equipment—part 2: particular requirements for the safety of magnetic resonance equipment for medical diagnosis.2002.International Electrotechnical CommissionGeneva, Switzerland 601–633
9. Collins C.M., Smith M.B.: Signal-to-noise ratio and absorbed power as functions of main magnetic field strength, and definition of “90 degrees” RF pulse for the head in the birdcage coil. Magn Reson Med 2001; 45: pp. 684-691.
10. von Klitzing L.: Do static magnetic fields of NMR influence biological signals?. Clin Phys Physiol Meas 1986; 7: pp. 157-160.
11. Hong C.Z., Shellock F.G.: Short-term exposure to a 1.5 Tesla static magnetic field does not affect somato-sensory-evoked potentials in man. Magn Reson Imaging 1990; 8: pp. 65-69.
12. Müller S., Hotz M.: Human brainstem auditory evoked potentials (BAEP) before and after MR examinations. Magn Reson Med 1990; 16: pp. 476-480.
13. Pacini S., Vannelli G.B., Barni T., et. al.: Effect of 0.2 T static magnetic field on human neurons: remodeling and inhibition of signal transduction without genome instability. Neurosci Lett 1999; 267: pp. 185-188.
14. Formica D., Silvestri S.: Biological effects of exposure to magnetic resonance imaging: an overview. Biomed Eng Online 2004; 3: pp. 11.
15. Rothwell J.C.: Techniques and mechanisms of action of transcranial stimulation of the human motor cortex. J Neurosci Methods 1997; 74: pp. 113-122.
16. Ziemann U., Lonnecker S., Steinhoff B.J., et. al.: Effects of antiepileptic drugs on motor cortex excitability in humans: a transcranial magnetic stimulation study. Ann Neurol 1996; 40: pp. 367-378.
17. Cantello R., Gianelli M., Civardi C., et. al.: Magnetic brain stimulation: the silent period after the motor evoked potential. Neurology 1992; 42: pp. 1951-1959.
18. Chen R., Lozano A.M., Ashby P.: Mechanism of the silent period following transcranial magnetic stimulation. Evidence from epidural recordings. Exp Brain Res 1999; 128: pp. 539-542.
19. Werhahn K.J., Kunesch E., Noachtar S., et. al.: Differential effects on motorcortical inhibition induced by blockade of GABA uptake in humans. J Physiol 1999; 517: pp. 591-597.
20. Chakeres D.W., Bornstein R., Kangarlu A.: Randomized comparison of cognitive function in humans at 0 and 8 Tesla. J Magn Reson Imaging 2003; 18: pp. 342-345.
21. Chakeres D.W., Kangarlu A., Boudoulas H., et. al.: Effect of static magnetic field exposure of up to 8 Tesla on sequential human vital sign measurements. J Magn Reson Imaging 2003; 18: pp. 346-352.
22. Schaefer D.J., Bourland J.D., Nyenhuis J.A.: Review of patient safety in time-varying gradient fields. J Magn Reson Imaging 2000; 12: pp. 20-29.
23. Bourland J.D., Nyenhuis J.A., Schaefer D.J.: Physiologic effects of intense MR imaging gradient fields. Neuroimaging Clin North Am 1999; 9: pp. 363-377.
24. Ham C.L., Engels J.M., van de Wiel G.T., et. al.: Peripheral nerve stimulation during MRI: effects of high gradient amplitudes and switching rates. J Magn Reson Imaging 1997; 7: pp. 933-937.
25. Scheef L., Landsberg M.W., Boecker H.: Methodological aspects of functional neuroimaging at high field strength: a critical review [article in German]. Rofo 2007; 179: pp. 925-931.
26. Shellock F.G., Schaefer D.J., Kanal E.: Physiologic responses to an MR imaging procedure performed at a specific absorption rate of 6.0 W/kg. Radiology 1994; 192: pp. 865-868.
27. Bestmann S.: The physiological basis of transcranial magnetic stimulation. Trends Cogn Sci 2008; 12: pp. 81-83.
28. Filipovic S.R., Siebner H.R., Rowe J.B., et. al.: Modulation of cortical activity by repetitive transcranial magnetic stimulation (rTMS): a review of functional imaging studies and the potential use in dystonia. Adv Neurol 2004; 94: pp. 45-52.
29. Arthurs O.J., Boniface S.: How well do we understand the neural origins of the fMRI BOLD signal?. Trends Neurosci 2002; 25: pp. 27-31.
30. Shibasaki H.: Human brain mapping: hemodynamic response and electrophysiology. Clin Neurophysiol 2008; 119: pp. 731-743.