Rationale and Objectives
To determine whether quantitative dynamic contrast-enhanced (DCE) and diffusion-weighted (DW) magnetic resonance imaging (MRI) features can discriminate malignant from benign axillary lymph nodes (ALNs) identified as suspicious on clinical breast MRI in patients newly diagnosed with breast cancer.
Materials and Methods
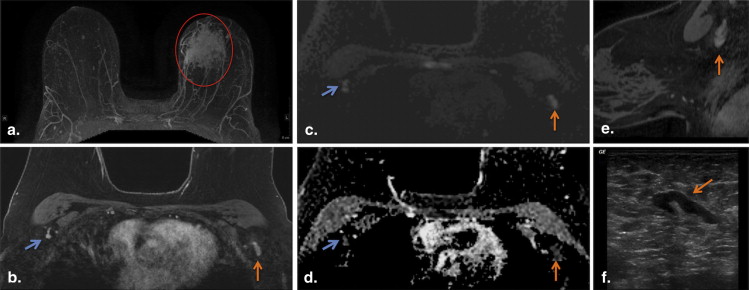
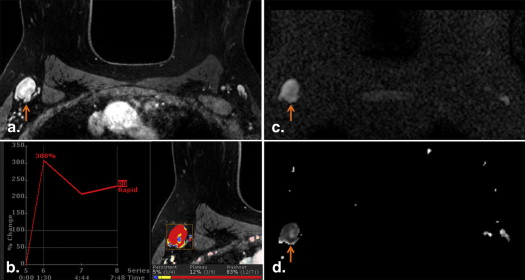
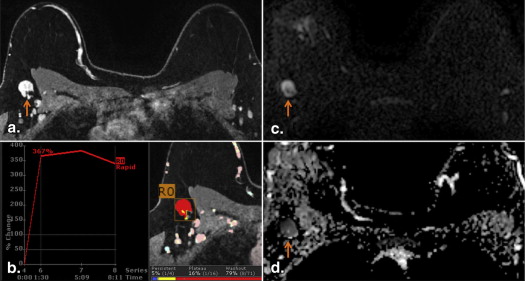
After approval from institutional review board, all clinical breast MR examinations performed from March 2006 through January 2010 describing at least one morphologically suspicious ipsilateral ALN in patients with newly diagnosed breast cancer were identified. Each suspicious ALN underwent ultrasound-guided core needle biopsy, and nodes with benign results were subsequently sampled surgically. Quantitative DCE and DW MRI parameters (diameters, volume, enhancement kinetics, and apparent diffusion coefficients [ADC]) were measured for each suspicious ALN and a representative contralateral normal node, and each feature was compared between the ALN groups (normal, benign, and malignant).
Results
Thirty-four suspicious ALNs (18 malignant and 16 benign) and 34 contralateral normal-appearing ALNs were included. Suspicious malignant and benign nodes exhibited larger size, greater volume, and lower ADCs than normal ALNs ( P < .05). Among suspicious ALNs, the only quantitative measure that discriminated between malignant from benign outcome was percent of ALN demonstrating washout kinetics ( P = .02).
Conclusions
In ALNs deemed morphologically suspicious on breast MRI, quantitative MRI features show little value in identifying those with malignant etiology.
Axillary lymph node (ALN) status in patients newly diagnosed with invasive breast cancer provides vital prognostic information to guide therapy. In clinically node-negative women with T1 or T2 invasive breast cancer, determination of ALN status has evolved from routine surgical removal of all level I and II ALNs with complete axillary lymph node dissection (ALND) to the modern practice of selective surgical sampling of a few (typically less than five) level I ALNs to exclude the presence of axillary nodal metastases with sentinel lymph node biopsy (SLNB). This less-invasive strategy results in completion ALND in only those patients with SLNB-proven lymph node metastases, has proven to be highly accurate, and allows most patients to avoid ALND and its associated high rate of morbidity . The use of ALND is expected to decline further since recent data from the American College of Surgery Oncology Group (ACOSOG) Z0011 trial showed a lack of survival or locoregional recurrence benefit of completion ALND in clinically node-negative but SLNB-positive women .
Although surgical evaluation of the axilla continues to trend toward less-extensive operations, the role of imaging in axillary assessments needs to evolve with surgical technique accordingly. Several recent studies have suggested breast magnetic resonance imaging (MRI) features of ALNs , and breast primary malignancies may hold promise to confirm the presence or absence of metastatic ALNs. Because breast MRI is increasingly being used at centers for preoperative evaluation of patients newly diagnosed with breast cancer, this potential added benefit is appealing . However, given new trends in management of the axilla in the post-ACOSOG Z0011 era, determining the presence of one or more ALN metastases that are not clinically suspicious but are detected solely by imaging may provide less clinical utility than determining the number of disease-laden ALNs by SLNB. Thus, we sought to assess the ability of quantitative dynamic contrast-enhanced (DCE) and diffusion-weighted (DW) MRI features to improve the positive predictive value (PPV) of clinical breast MRI assessments of morphologically suspicious ALNs using direct pathology-to-imaging verification.
Materials and methods
Get Radiology Tree app to read full this article<
Patient Population
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
MRI Technique
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Image Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
(4/3π×abc)8 (
4
/
3
π
×
abc
)
8
where a, b, and c are the three orthogonal diameters (AP, ML, and SI).
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
ADC=−(1b)ln(SDWIS0) ADC
=
−
(
1
b
)
ln
(
S
DWI
S
0
)
where b = 600 s/mm 2 , S DWI is the combined DW image (geometric average of individual b = 600 s/mm 2 DW images), and S 0 is the b = 0 s/mm 2 reference image.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Ratio=[suspiciousALNvalue][normalALNvalue] Ratio
=
[
suspicious
ALN
value
]
[
normal
ALN
value
]
where ratio is the intrapatient ratio for a given MRI parameter, suspicious ALN value is the measured value for that MRI parameter for a given patient, and normal ALN value is the measured value for that MRI parameter for the same patient.
Get Radiology Tree app to read full this article<
ALN Ultrasound CNB Technique
Get Radiology Tree app to read full this article<
Histopathology
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 1
Index Tumor Characteristics for All Patients Included in the Study
Characteristic Benign ALN ( N = 16) Malignant ALN ( N = 18) Total ( N = 34) Maximum tumor size, mm; median (range) 17 (9–45) 18 (11–29) 17 (9–45) Tumor histology, n (%) DCIS 1 (6.3) 0 (0) 1 (2.9) IDC 13 (81.3) 15 (83.3) 28 (82.4) ILC 1 (6.3) 3 (16.7) 4 (11.8) Poorly differentiated carcinoma 1 (6.3) 0 (0) 1 (2.9) Nottingham Score, n (%) 1 2 (12.5) 2 (11.1) 4 (11.8) 2 5 (32.3) 6 (33.3) 11 (32.4) 3 7 (43.8) 10 (55.6) 17 (50.0) Not assessed (DCIS and poorly differentiated carcinoma) 2 (12.5) 0 (0) 2 (5.6) Estrogen receptor, n (%) Positive 6 (37.5) 12 (66.7) 18 (52.9) Negative 9 (56.3) 6 (33.3) 15 (44.1) Unknown 1 (6.3) 0 (0) 1 (2.9) Progesterone receptor, n (%) Positive 4 (25.0) 11 (61.1) 15 (44.1) Negative 9 (56.3) 7 (38.9) 16 (47.1) Unknown 3 (19.0) 0 (0) 3 (8.8) HER2/neu receptor, n (%) Positive 0 (0) 3 (16.7) 3 (8.8) Negative 12 (75.0) 14 (77.8) 26 (76.5) Unknown 4 (25.0) 1 (2.6) 5 (14.7) Ki-67 (%), mean (range) 53.8 (5–90) 38 (5–80) 45.4 (5–90)
DCIS, ductal carcinoma in situ; IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Suspicious Malignant Outcome Versus Normal ALN Comparisons
Get Radiology Tree app to read full this article<
Table 2
Comparison of Quantitative MRI Features of Malignant Versus Contralateral Normal Axillary Lymph Nodes (ALNs) in 34 Patients with Breast Cancer
Feature Malignant ALN, mean (SD) Normal ALN, mean (SD)P Value Kinetic features Peak enhancement (%) 440.6 (299.0) 324.8 (226.9) .11 Washout (%) 73.4 (20.9) 72.4 (20.7) .80 Size Angiographic volume (mm 3 ) 1.8 (1.9) 0.4 (0.3) <.0001 ∗ Manual volume (mm 3 ) 2.0 (1.7) 0.4 (0.3) <.0001 ∗ Maximum size (mm) 19.4 (5.2) 12.6 (5.7) .0008 ∗ Minimum size (mm) 10.6 (3.2) 5.7 (2.1) <.0001 ∗ DW MRI features Mean ADC (mm 2 /s) 1.01 (0.2) 1.14 (0.2) .02 ∗ Minimum ADC (mm 2 /s) 0.51 (0.2) 0.73 (0.3) .002 ∗
ADC, apparent diffusion coefficient; DW, diffusion weighted; MRI, magnetic resonance imaging; SD, standard deviation.
P values were calculated by Wilcoxon signed rank test.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Suspicious Benign Outcome Versus Normal ALN Comparisons
Get Radiology Tree app to read full this article<
Table 3
Comparison of Quantitative MRI Features of Benign Versus Contralateral Normal Axillary Lymph Nodes (ALNs) in 34 Patients with Breast Cancer
Feature Benign ALN, mean (SD) Normal ALN, mean (SD)P Value Kinetic features Peak enhancement (%) 398.7 (225.9) 411.7 (470.7) .38 Washout (%) 88.4 (12.8) 82.8 (16.8) .4 Size Angiographic volume (mm 3 ) 3.2 (4.5) 0.5 (0.6) .001 ∗ Manual volume (mm 3 ) 3.5 (5.9) 0.8 (0.7) .0002 ∗ Maximum size (mm) 20.7 (9.9) 14.9 (6.3) .06 Minimum size (mm) 12.5 (5.3) 6.8 (2.8) <.0001 ∗ DW MRI features Mean ADC (mm 2 /s) 1.03 (0.2) 1.12 (0.2) .08 Minimum ADC (mm 2 /s) 0.44 (0.2) 0.69 (0.3) .003 ∗
ADC, apparent diffusion coefficient; DW, diffusion weighted; MRI, magnetic resonance imaging; SD, standard deviation.
P values were calculated by Wilcoxon signed rank test.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Suspicious Malignant Outcome Versus Benign Outcome ALN Comparisons
Get Radiology Tree app to read full this article<
Table 4
Comparison of Quantitative MRI Features between Benign and Malignant Morphologically Suspicious Axillary Lymph Nodes (ALNs)
Feature Benign ALN, mean (SD) Malignant ALN, mean (SD)P Value Kinetic features Peak enhancement (%) 398.7 (225.9) 440.6 (299.0) .63 Washout (%) 88.4 (12.8) 73.4 (20.9) .03 ∗ Size Angiographic volume (mm 3 ) 3.2 (4.5) 1.8 (1.9) .68 Manual volume (mm 3 ) 3.5 (5.9) 2.0 (1.7) .61 Maximum size (mm) 20.7 (9.9) 19.4 (5.2) .96 Minimum size (mm) 12.5 (5.3) 10.6 (3.2) .30 DW MRI features Mean ADC (mm 2 /s) 1.03 (0.2) 1.01 (0.2) .62 Minimum ADC (mm 2 /s) 0.44 (0.2) 0.5 (0.2) .39
ADC, apparent diffusion coefficient; DW, diffusion weighted; MRI, magnetic resonance imaging; SD, standard deviation.
P values were calculated by Mann–Whitney U test.
Get Radiology Tree app to read full this article<
Table 5
Comparison of Intraindividual Normalized Quantitative MRI Features between Benign and Malignant Morphologically Suspicious Axillary Lymph Nodes (ALN)
Feature Benign ALN, mean (SD) Malignant ALN, mean (SD)P Value Kinetic feature ratios Peak enhancement 1.43 (1.3) 2.0 (2.4) .26 Washout 1.12 (0.3) 1.11 (0.5) .96 Size ratios Angiographic volume ratio 1.17 (1.6) 1.05 (1.2) .77 Manual volume ratio 4.96 (5.0) 9.38 (16.4) .15 Maximum size 1.52 (0.7) 1.91 (1.3) .39 Minimum size 1.95 (0.7) 1.99 (0.8) .93 DW MRI feature ratios Mean ADC ratio 0.95 (0.2) 0.90 (0.2) .40 Minimum ADC ratio 0.70 (0.4) 0.85 (0.8) .99
ADC, apparent diffusion coefficient; DW, diffusion weighted; MRI, magnetic resonance imaging; SD, standard deviation.
All values are ratios of suspicious ALN-to-contralateral normal ALN, and thus, there are no units.
P values were calculated by Wilcoxon rank sum test.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Martin R.C., Chagpar A., Scoggins C.R., et. al.: Clinicopathologic factors associated with false-negative sentinel lymph-node biopsy in breast cancer. Ann Surg 2005; 241: pp. 1005-1012. discussion 12–5
2. Veronesi U., Paganelli G., Viale G., et. al.: A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med 2003; 349: pp. 546-553.
3. Giuliano A.E., Hunt K.K., Ballman K.V., et. al.: Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 2011; 305: pp. 569-575.
4. He N., Xie C., Wei W., et. al.: A new, preoperative, MRI-based scoring system for diagnosing malignant axillary lymph nodes in women evaluated for breast cancer. Eur J Radiol 2012; 81: pp. 2602-2612.
5. Junping W., Tongguo S., Yunting Z., et. al.: Discrimination of axillary metastatic from nonmetastatic lymph nodes with PROPELLER diffusion-weighted MR imaging in a metastatic breast cancer model and its correlation with cellularity. J Magn Reson Imaging 2012; 36: pp. 624-631.
6. Kamitani T., Hatakenaka M., Yabuuchi H., et. al.: Detection of axillary node metastasis using diffusion-weighted MRI in breast cancer. Clin Imaging 2013; 37: pp. 56-61.
7. Luo N., Su D., Jin G., et. al.: Apparent diffusion coefficient ratio between axillary lymph node with primary tumor to detect nodal metastasis in breast cancer patients. J Magn Reson Imaging 2013; 38: pp. 824-828.
8. Scaranelo A.M., Eiada R., Jacks L.M., et. al.: Accuracy of unenhanced MR imaging in the detection of axillary lymph node metastasis: study of reproducibility and reliability. Radiology 2012; 262: pp. 425-434.
9. Loiselle C., Eby P.R., Kim J.N., et. al.: Preoperative MRI improves prediction of extensive occult axillary lymph node metastases in breast cancer patients with a positive sentinel lymph node biopsy. Acad Radiol 2014; 21: pp. 92-98.
10. Lehman C.D., DeMartini W., Anderson B.O., et. al.: Indications for breast MRI in the patient with newly diagnosed breast cancer. J Natl Compr Canc Netw 2009; 7: pp. 193-201.
11. Lehman C.D., Gatsonis C., Kuhl C.K., et. al.: MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N Engl J Med 2007; 356: pp. 1295-1303.
12. Mortellaro V.E., Marshall J., Singer L., et. al.: Magnetic resonance imaging for axillary staging in patients with breast cancer. J Magn Reson Imaging 2009; 30: pp. 309-312.
13. Rahbar H., Partridge S.C., Javid S.H., et. al.: Imaging axillary lymph nodes in patients with newly diagnosed breast cancer. Curr Probl Diagn Radiol 2012; 41: pp. 149-158.
14. Krammer J., Engel D., Nissen J., et. al.: Characteristics of axillary lymph nodes apparent on dynamic contrast-enhanced breast MRI in healthy women. Clin Imaging 2012; 36: pp. 249-254.
15. Partridge S.C., Rahbar H., Murthy R., et. al.: Improved diagnostic accuracy of breast MRI through combined apparent diffusion coefficients and dynamic contrast-enhanced kinetics. Magn Reson Med 2011; 65: pp. 1759-1767.
16. Amersi F., Giuliano A.E.: Management of the axilla. Hematol Oncol Clin North Am 2013; 27: pp. 687-702.
17. Murray A.D., Staff R.T., Redpath T.W., et. al.: Dynamic contrast enhanced MRI of the axilla in women with breast cancer: comparison with pathology of excised nodes. Br J Radiol 2002; 75: pp. 220-228.
18. Valente S.A., Levine G.M., Silverstein M.J., et. al.: Accuracy of predicting axillary lymph node positivity by physical examination, mammography, ultrasonography, and magnetic resonance imaging. Ann Surg Oncol 2012; 19: pp. 1825-1830.
19. Kvistad K.A., Rydland J., Smethurst H.B., et. al.: Axillary lymph node metastases in breast cancer: preoperative detection with dynamic contrast-enhanced MRI. Eur Radiol 2000; 10: pp. 1464-1471.
20. Baltzer P.A., Dietzel M., Burmeister H.P., et. al.: Application of MR mammography beyond local staging: is there a potential to accurately assess axillary lymph nodes? Evaluation of an extended protocol in an initial prospective study. AJR Am J Roentgenol 2011; 196: pp. W641-W647.
21. Fornasa F., Nesoti M.V., Bovo C., et. al.: Diffusion-weighted magnetic resonance imaging in the characterization of axillary lymph nodes in patients with breast cancer. J Magn Reson Imaging 2012; 36: pp. 858-864.
22. Demartini W.B., Rahbar H.: Breast magnetic resonance imaging technique at 1.5 t and 3 t: requirements for quality imaging and American College of Radiology accreditation. Magn Reson Imaging Clin N Am 2013; 21: pp. 475-482.
23. Rahbar H., Partridge S.C., DeMartini W.B., et. al.: Clinical and technical considerations for high quality breast MRI at 3 Tesla. J Magn Reson Imaging 2013; 37: pp. 778-790.