Purpose
To evaluate the performance of T2 star-weighted angiography (SWAN) to concomitantly assess the prostate contour while detecting fiducials before magnetic resonance (MR)-based intensity-modulated radiation therapy (IMRT) in prostate carcinoma.
Materials and Methods
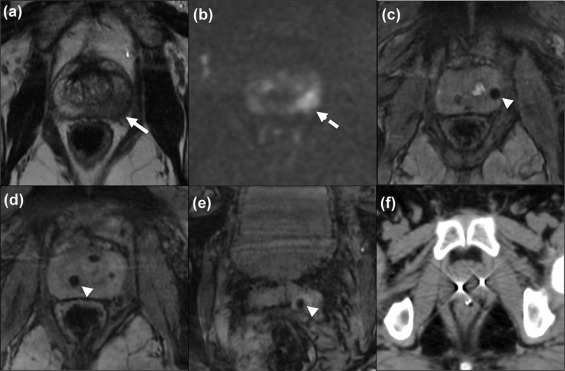
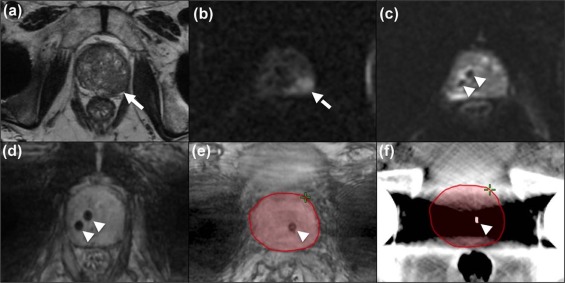
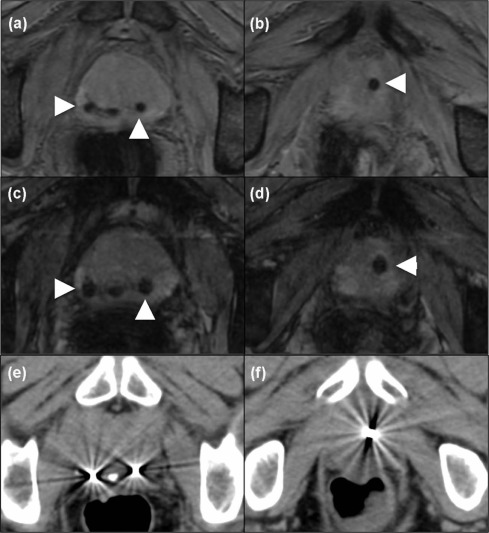
Forty patients (mean age: 73.1 ± 7.5 years; average Gleason score: 7 ± 1; average prostate-specific antigen: 14.7 ± 11.6 ng/mL) underwent MR and computed tomography imaging before fiducial-based IMRT. MR protocol included SWAN, T2-weighted (T2w) and diffusion-weighted imaging in a first group ( n = 20) and SWAN, T2w and T2-star weighted imaging in a second group ( n = 20). In group 1, the depiction of fiducials, image sharpness and visibility of prostate boundaries were independently evaluated by 2 readers on SWAN, T2w or diffusion-weighted images. In group 2, a similar evaluation was performed by 2 other readers on SWAN and T2-star images only. Depiction of fiducials was compared to computed tomography findings.
Results
The median scores of visibility of prostate boundaries, image sharpness and depiction of fiducials by SWAN were above average to excellent for all readers. In group 1, readers correctly located 56 of 57 (98.2%) and 47 of 57 (82.5%) fiducials, respectively; and 50 of 51 (98%), and 48 of 51 (88.2%) fiducials in group 2, respectively.
Conclusion
By allowing adequate visualization of the prostate boundaries and high depiction of fiducial markers concomitantly, SWAN might be used for treatment planning of IMRT. The use of this sequence might simplify the registration process and limit any errors associated with image fusion.
Introduction
Intensity-modulated radiotherapy (IMRT) in prostate carcinoma may potentially improve outcomes by creating sharp borders confining high dose to the prostate and leading to spare the surrounding organs . However, IMRT requires improved evaluation of the prostatic gland to individually determine the optimal treatment plan . To overcome the traditional limitations of computed tomography (CT)-based IMRT workflow, fiducial markers have been used to enable landmark-based alignment of magnetic resonance images (MRI) to the planning CT images . This CT-MR combination allows accurate registration and mapping of the prostate contour, leading to accurate dose delivery.
The MR protocol performed before MR-based IMRT usually includes a T2 star-weighted sequence helping to identify the fiducials as well as a pT2-weighted (T2w) sequence to delineate the prostate contour . Multi-echo gradient-recalled echo (GRE) T2 star-weighted imaging provides better detection of implanted fiducial markers when compared to both fast spin-echo and single-echo GRE T2w imaging but gives relatively poor anatomic localization . To address these both priorities in the same sequence, T2 star-weighted angiography (SWAN) is highly sensitive to differences in magnetic susceptibility and provides a clear, high-resolution three-dimensional (3D) dataset, integrating a broad range of distinct tissue contrasts allowing to visualize anatomic structures . SWAN applies a multi-time-to-echo readout technique that generates a high signal-to-noise ratio and appears less affected by the chemical shift compared to other susceptibility-weighted imaging techniques. Moreover, SWAN helps to delineate small blood vessels, microbleeds, and large vascular structures but also iron and calcium deposits, as reported in the brain . We hypothesized that MR protocols including SWAN might permit accurate MR-based treatment planning by allowing both visualization of the whole prostate anatomy and the fiducials . The aim of this preliminary study was therefore to evaluate the performance of SWAN to concomitantly assess the prostate contour while detecting fiducials before MR-based IMRT in prostate carcinoma.
Materials and Methods
Get Radiology Tree app to read full this article<
Patients
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Magnetic Resonance Imaging Protocol
Get Radiology Tree app to read full this article<
TABLE 1
Magnetic Resonance Imaging Protocol
T2-weighted
Cube 3DFSE Diffusion-weighted
SE EPI T2 Star-weighted Angiography
(SWAN) EFGRE3D Multiple-echo Recombined Gradient Echo (MERGE) Imaging plane Axial Axial Axial Axial Acquisition 3D 2D 3D 3D Field of view (mm) 240 300 280 280 TR/TE eff (ms) 2800/110 5400/90 42/24 30/12 Echo train length 78 1 6 4 Flip angle 90 90 15 10 Matrix size 320/288 140/200 320/288 224/288 Receiver bandwidth (Hz/voxel) 62.50 62.50 62.50 41.67 Slice thickness/gap (mm) 1.4 4.0 2.8 2.0 N o of excitations 1 — 1 1 Acceleration factor — — — — Acquisition time (min) 5.48 3.25 2.08 3.10 b Value (mm2/s) — 0; 2000 — —
3DFSE, 3-dimensional fast spin-echo; EFGRE3D, Enhanced Fast GRadient Echo 3-Dimensional; SE EPI, spin-echo echo-planar imaging.
Get Radiology Tree app to read full this article<
Visual and Statistical Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Image Quality and Interobserver Agreement
Get Radiology Tree app to read full this article<
TABLE 2
Qualitative Assessments of MR Images in Group 1 (20 Patients)
Reader 1 Reader 2 T2W DWI SWAN T2W DWI SWAN Identification of the prostate boundaries 5
[4–5] 3
[3–4] 4
[3–5] 4
[4–5] 2
[2–3] 5
[5–5] Image sharpness 4
[3.5–5] 3
[2–4] 3
[2–3] 4
[3–4.5] 4
[3.5–4] 4
[2.5–5] Depiction of fiducials 1
[1–1] 3
[2–3] 5
[4–5] 1
[1–1] 1
[1–1] 5
[5–5]
DWI, diffusion-weighted images; MR, magnetic resonance; SWAN, T2 star-weighted angiography; T2W, T2-weighted images.
All data are expressed as median [interquartile range].
TABLE 3
Qualitative Assessments of MR Images in Group 2 (20 Patients)
Reader 3 Reader 4 MERGE SWAN MERGE SWAN Identification of the prostate boundaries 5
[5–5] 5
[3.75–5] 5
[3–5] 4
[3–4] Image sharpness 5
[4.75–5] 4
[3–4.25] 5
[3–5] 4
[4–4] Depiction of fiducials 5
[5–5] 5
[4–5] 5
[3–5] 5
[5–5]
MERGE, multiple-echo recombined gradient echo; MR, magnetic resonance; SWAN, T2 star-weighted angiography.
All data are expressed as median [interquartile range].
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Prostate Volume Analysis
Get Radiology Tree app to read full this article<
TABLE 4
Prostate Volume
Group 1 ( n = 60) Group 2 ( n = 60) Reader 1 Reader 2 Reader 3 Reader 4 T2W 34.54
[23.16–41.07] 34
[26.85–47.7] 39.07
[29.4–62.05] 34.07
[24.71–56.1] SWAN 35.44
[22.07–49.24] 37.15
[25.3–52.3] 36.83
[27.82–66.40] 28.42
[22–39.87]
SWAN, T2 star-weighted angiography; T2W, T2-weighted images.
All data are expressed as median [interquartile range] and in cm 3 .
Get Radiology Tree app to read full this article<
Depiction of Fiducials
Get Radiology Tree app to read full this article<
TABLE 5
Number of Fiducials Adequately Detected in the Prostate
Group 1 ( n = 60) Group 2 ( n = 60) Reader 1 Reader 2 Reader 3 Reader 4 CT scan 57 57 51 51 SWAN 56
(98.2%) 47
(82.5%) 50
(98%) 48
(88.2%) MERGE — — 51
(100%) 44
(86.3%)
CT, computed tomography; MERGE, multiple-echo recombined gradient echo; SWAN, T2 star-weighted angiography.
For each patient, three fiducials were introduced in the prostate under ultrasound guidance. The total of fiducials inserted in patients was 60 for each group. In group 1, three fiducials were located outside the prostate, and nine in group 2 as assessed by CT scan.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgment
Get Radiology Tree app to read full this article<
References
1. Mohler J.L., Kawachi M.H., Bahnson R.R., et. al.: The 2010 NCCN clinical practice guidelines in oncology on prostate cancer. J Natl Compr Canc Netw 2010; 8: pp. 162-200.
2. Boonsirikamchai P., Choi S., Frank S.J., et. al.: MR imaging of prostate cancer in radiation oncology: what radiologists need to know. Radiographics 2013; 33: pp. 741-761.
3. Arrayeh E., Westphalen A.C., Kurhanewicz J., et. al.: Does local recurrence of prostate cancer after radiation therapy occur at the site of primary tumor? Results of a longitudinal MRI and MRSI study. Int J Radiat Oncol Biol Phys 2012; 82: pp. e787-e793.
4. Valerio M., Ahmed H.U., Emberton M., et. al.: The role of focal therapy in the management of localised prostate cancer: a systematic review. Eur Urol 2014; 66: pp. 732-751.
5. Barret E., Ahallal Y., Sanchez-Salas R., et. al.: Morbidity of focal therapy in the treatment of localized prostate cancer. Eur Urol 2013; 63: pp. 618-622.
6. Soylu F.N., Peng Y., Jiang Y., et. al.: Seminal vesicle invasion in prostate cancer: evaluation by using multiparametric endorectal MR imaging. Radiology 2013; 267: pp. 797-806.
7. Feathers D.J., Rollings K., Hedge A.: Alternative computer mouse designs: performance, posture, and subjective evaluations for college students aged 18–25. Work 2013; 44: pp. S115-S122.
8. Schieda N., Avruch L., Shabana W.M., et. al.: Multi-echo gradient recalled echo imaging of the pelvis for improved depiction of brachytherapy seeds and fiducial markers facilitating radiotherapy planning and treatment of prostatic carcinoma. J Magn Reson Imaging 2015; 41: pp. 715-720.
9. Chen L., Price R.A., Wang L., et. al.: MRI-based treatment planning for radiotherapy: dosimetric verification for prostate IMRT. Int J Radiat Oncol Biol Phys 2004; 60: pp. 636-647.
10. Nagahama H., Suzuki K., Shonai T., et. al.: Comparison of magnetic resonance imaging sequences for depicting the subthalamic nucleus for deep brain stimulation. Radiol Phys Technol 2015; 8: pp. 30-35.
11. Boeckh-Behrens T., Lutz J., Lummel N., et. al.: Susceptibility-weighted angiography (SWAN) of cerebral veins and arteries compared to TOF-MRA. Eur J Radiol 2012; 81: pp. 1238-1245.
12. Wu Z., Mittal S., Kish K., et. al.: Identification of calcification with MRI using susceptibility-weighted imaging: a case study. J Magn Reson Imaging 2009; 29: pp. 177-182.
13. Rosenkrantz A.B., Kim S., Lim R.P., et. al.: Prostate cancer localization using multiparametric MR imaging: comparison of prostate imaging reporting and data system (PI-RADS) and Likert scales. Radiology 2013; 269: pp. 482-492.
14. Donati O.F., Afaq A., Vargas H.A., et. al.: Prostate MRI: evaluating tumor volume and apparent diffusion coefficient as surrogate biomarkers for predicting tumor Gleason score. Clin Cancer Res 2014; 20: pp. 3705-3711.
15. Vargas H.A., Hotker A.M., Goldman D.A., et. al.: Updated prostate imaging reporting and data system (PIRADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. Eur Radiol 2016; 26: pp. 1606-1612.
16. Turkbey B., Choyke P.L.: PIRADS 2.0: what is new?. Diagn Interv Radiol 2015; 21: pp. 382-384.
17. Haas M., Gunzel K., Miller K., et. al.: Is the ellipsoid formula the new standard for 3-tesla MRI prostate volume calculation without endorectal coil?. Urol Int 2017; 98: pp. 49-53.
18. Barentsz J.O., Richenberg J., Clements R., et. al.: ESUR prostate MR guidelines 2012. Eur Radiol 2012; 22: pp. 746-757.
19. Hodel J., Leclerc X., Khaled W., et. al.: Comparison of 3D multi-echo gradient-echo and 2D T2* MR sequences for the detection of arterial thrombus in patients with acute stroke. Eur Radiol 2014; 24: pp. 762-769.
20. Cassidy R.J., Yang X., Liu T., et. al.: Neurovascular bundle-sparing radiotherapy for prostate cancer using MRI-CT registration: a dosimetric feasibility study. Med Dosim 2016; 41: pp. 339-343.
21. Bosemani T., Verschuuren S.I., Poretti A., et. al.: Pitfalls in susceptibility-weighted imaging of the pediatric brain. J Neuroimaging 2014; 24: pp. 221-225.
22. Heijmink S.W., Scheenen T.W., van Lin E.N., et. al.: Changes in prostate shape and volume and their implications for radiotherapy after introduction of endorectal balloon as determined by MRI at 3T. Int J Radiat Oncol Biol Phys 2009; 73: pp. 1446-1453.
23. De Brabandere M., Hoskin P., Haustermans K., et. al.: Prostate post-implant dosimetry: interobserver variability in seed localisation, contouring and fusion. Radiother Oncol 2012; 104: pp. 192-198.