Rationale and Objectives
To better prepare radiology residents for providing care within the context of the larger health care system, this study evaluated the feasibility and impact of a curriculum to enhance radiology residents’ understanding and ability to apply concepts from medical management and industrial and operational engineering to systems-based practice problems in radiology practice.
Materials and Methods
A multiprofessional team including radiology, medical education, and industrial and operational engineering professionals collaborated in developing a seven-module curriculum, including didactic lectures, interactive large-group analysis, and small-group discussions with case-based radiology examples, which illustrated real-life management issues and the roles physicians held. Residents and faculty participated in topic selection. Pre- and post-instruction formative assessments were administered, and results were shared with residents during teaching sessions.
Results
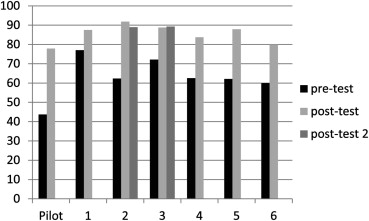
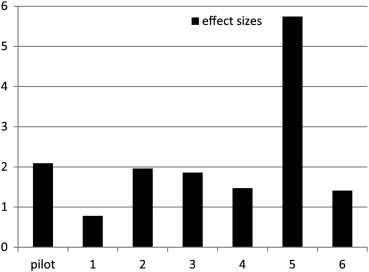
Attendance and participation in case-based scenario resolutions indicate the feasibility and impact of the interactive curriculum on residents’ interest and ability to apply curricular concepts to systems-based practice in radiology. Paired t test analyses ( P < .05) and effect sizes showed residents significantly increased their knowledge and ability to apply concepts to systems-based practice issues in radiology.
Conclusions
Our iterative curriculum development and implementation process demonstrated need and support for a multiprofessional team approach to teach management and operational engineering concepts. Curriculum topics are congruent with Accreditation Council for Graduate Medical Education requirements for systems-based practice. The case-based curriculum using a mixed educational format of didactic lectures and small-group discussion and problem analysis could be adopted for other radiology programs, for both residents and continuing medical education applications.
To increase residents’ understanding of health care systems so that physicians can initiate and lead improvements in health care delivery, the Accreditation Council for Graduate Medical Education (ACGME) introduced a mandate that residency programs provide training and assessment of resident competency in “systems-based practice” (SBP). As Graham et al caution, the ACGME provides a broad definition of SBP—“an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value”—but does not provide operational definitions or scope of practice for specific medical specialties .
Medical educators have stressed the value of formal resident training in SBP, drawing on principles and strategies from health care policy, management, and business to lead health care improvements . However, few residents have formal training in business or management principles before or during residency . Consequently, when faced with complex business and management decisions in health systems, they are unsure how to proceed, frame questions, and seek assistance.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and methods
Subjects
Get Radiology Tree app to read full this article<
Topic Selection
Get Radiology Tree app to read full this article<
Table 1
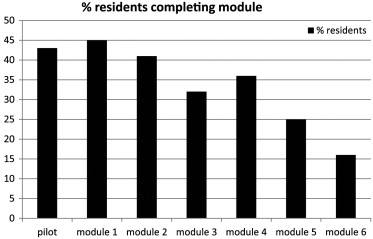
Description of Modules and Number of Residents Completing Module
Module # Module Title Module Description No. of Residents ∗ Pilot Costing Analysis Lack of financial metrics for management decision making and how to create them with costing analysis 19 1 Fundamentals of Improvement: The Quality Gap Methods and tools for quality management:
Plan-Do-Study-Act (PDSA) and lean process improvement approaches 20 2 Profiles of Practice Groups and Compensation Current radiology practice group sizes and patterns of hiring
Compensation: starting and partnership levels
Range of workloads and structures of practice 18 3 Group Governance and Merger: How to Select, Govern, and Thrive in Group Practice Organizational dynamics and governance issues presented as the culture of the corporation
How to recognize and adapt group culture in a competitive business environment 14 4 Data Collection: Partnering with Engineers: Techniques for Process Improvement in MR Examples from ongoing work with the Industrial and Operations Engineering Department
How to derive and communicate actionable data for process and quality improvement by gathering workplace observations 16 5 Fixing Health Care: Harvard Business Review April 2010 Issue Health care policy and economics through the business lens
National and worldwide data on the health care economics and business models 11 6 Negotiation and Conflict Management Negotiation and leadership strategies
Conflict management techniques applied to radiology examples 7
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Curriculum Development
Get Radiology Tree app to read full this article<
Table 2
Description of Module Topics and Associated Systems-Based Practice Resident Role
∗ Adapted with permission from Graham MJ, Naqvi Z, Encandela J, et al. Systems-based practice defined: taxonomy development and role identification for competency assessment of residents. J Grad Med Educ 2009; September:49–60.
Module # Title Systems-Based Practice (SBP) Resident Roles Pilot Costing Analysis Resource manager
System evaluator 1 Fundamentals of Improvement: The Quality Gap System evaluator
Patient advocate
Resource manager
Care coordinator 2 Profiles of Practice Groups and Compensation System consultant
Team collaborator 3 Group Governance and Merger: How to Select, Govern and Thrive in Group Practice System evaluator
Team collaborator 4 Data Collection: Partnering with Engineers: Techniques for Process Improvement in MR Resource manager
Care coordinator 5 Fixing Health Care: Harvard Business Review April 2010 Issue. System consultant
Resource manager
Team collaborator
Patient advocate 6 Negotiation and Conflict Management. Patient advocate
Team collaborator
System consultant
Get Radiology Tree app to read full this article<
Educational Intervention
Get Radiology Tree app to read full this article<
Assessment
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Curriculum Feasibility
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Assessment of Knowledge and Confidence
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Graham M.J., Naqvi Z., Encandela J., et. al.: Systems-based practice defined: Taxonomy development and role identification for competency assessment of residents. J Grad Med Educ 2009; September; pp. 49-60.
2. Chan S.: Management education during radiology residency: Development of an educational practice. Acad Radiol 2004; 11: pp. 1308-1317.
3. Mirowitz S.A.: Development and assessment of a radiology core curriculum in health care policy and practice. Acad Radiol 2000; 7: pp. 540-550.
4. Armstrong E.G., Mackey M., Spear S.J.: Medical education as a process management problem. Acad Med 2004; 79: pp. 721-728.
5. Duszak R., Muroff L.R.: Measuring and managing radiologist productivity, part 1: Clinical metrics and benchmarks. J Am Coll Radiol 2010; 7: pp. 452-458.
6. Steele J.R., Schomer D.F.: Continuous quality improvement programs provide new opportunities to drive value innovation initiatives in hospital-based radiology practices. J Am Coll Radiol 2009; 6: pp. 491-499.
7. Varkey P., Karlapudi S.P., Bennet K.E.: Teaching quality improvement: A collaboration project between medicine and engineering. Am J Med Qual 2008; 23: pp. 296-301.
8. Gunderman R.B., Tawadros A.M., Travison T.: Business education for radiology residents: The value of full-time business educators. Acad Radiol 2011; 18: pp. 645-649.
9. Kerfoot B.P., Conlin P.R., et. al.: Web-based education in systems-based practice: A randomized trial. Arch Intern Med 2007; 167: pp. 361-366.
10. Jenson H.B., Dorner D., Hinchey K., et. al.: Integrating quality improvement and residency education: Insights from the AIAMC National Initiative about the roles of the designated institutional official and program director. Acad Med 2009; 84: pp. 1749-1756.
11. Lurie S.J., Mooney C.J., Lyness J.M.: Measurement of the general competencies of the accreditation council for graduate medical education: A systematic review. Acad Med 2009; 84: pp. 301-309.
12. Colbert C., Ogden P., Ownby A., et. al.: Systems-based practice in graduate medical education: Systems thinking as the missing foundational construct. Teach Learn Med 2011; 23: pp. 179-185.
13. Wittich C.M., Reed D.A., McDonald F.S., et. al.: Perspective: Transformative learning: A framework using critical reflection to link the improvement competencies in graduate medical education. Acad Med 2010; 85: pp. 1790-1793.
14. Daniel D.M., Casey D.E., Levine J.L., et. al.: Taking a unified approach to teaching and implementing quality improvements across multiple residency programs: The Atlantic Health experience. Acad Med 2009; 84: pp. 1788-1795.
15. Holland R., Meyers D., Hildebrand C., et. al.: Creating champions for health care quality and safety. Am J Med Qual 2010; 25: pp. 102-108.
16. Voss J.D., May N.B., Schorling J.B., et. al.: Changing conversations: Teaching safety and quality in residency training. Acad Med 2008; 83: pp. 1080-1087.
17. Wong B.M., Etchells E.E., Kuper A., et. al.: Teaching quality improvement and patient safety to trainees: A systematic review. Acad Med 2010; 85: pp. 1425-1439.
18. 2005 Association of Program Directors in Radiology (APDR) annual survey results. Available at: http://www.apdr.org/sitemap.cfm . Accessed July 27, 2012.
19. Amis E.S.: New program requirements for diagnostic radiology: Update and discussion of the more complex requirements. AJR Am J Roentgenol 2008; 190: pp. 2-4.
20. Brandon C.J., Holody M., Inch G., et. al.: Partnering with engineers to identify and empirically evaluate delays in magnetic resonance imaging laying the foundations for quality improvement and system-based practice in radiology. Acad Radiol 2012; 19: pp. 109-115.
21. Reid P.P., Compton W.D., Grossman J.H., et. al.: Building a better delivery system: A new engineering/health care partnership.2005.National Academies PressWashington, DC
22. Lynch D.C., Johnson J.J.: A separate-sample pretest-post-test design to evaluate a practice-management seminar for residents. Acad Med 1999; 74: pp. 605-606.
23. Hojat M., Xu G.: A visitor’s guide to effect sizes: Statistical significance versus practical (clinical) importance of research findings. Adv Health Sci Educ Theory Pract 2004; 9: pp. 241-249.
24. Earnest M., Wong S.L., Federico S.G.: Perspective: Physician advocacy: What is it and how do we do it?. Acad Med 2010; 85: pp. 63-67.
25. Kern D.E., Thomas P.A., Howard D.H., et. al.: Curriculum development for medical education: A six-step approach.1998.The Johns Hopkins University PressBaltimore, MD
26. Kruskal J.B., Anderson S., Yam C.S., et. al.: Strategies for establishing a comprehensive quality and performance improvement program in a radiology department. Radiographics 2009; 29: pp. 315-329.
27. Johnson C.D., Krecke K.N., Miranda R., et. al.: Quality initiatives: Developing a radiology quality and safety program: A primer. Radiographics 2009; 29: pp. 951-959.
28. Panek R.C., Deloney L.A., Park J., et. al.: Interdepartmental problem-solving as a method for teaching and learning systems-based practice. Acad Radiol 2006; 13: pp. 1150-1154.
29. Ziegelstein R.C., Fiebach N.H.: “The mirror” and “the village”: A new method for teaching practice-based learning and improvement and systems-based practice. Acad Med 2004; 79: pp. 83-88.
30. Otero Hansel J., Weissman B.N., Rybicki F.J.: System-based practice: Proposal for a comprehensive curriculum. Acad Radiol 2008; 15: pp. 119-126.
31. Relyea-Chew A., Talner L.: A dedicated general competencies curriculum for radiology residents: Development and implementation. Acad Radiol 2011; 18: pp. 650-654.
32. Krajewshi K., Siewert B., Yam S., et. al.: A quality assurance elective for radiology residents. Acad Radiol 2007; 41: pp. 239-245.
33. Buchmann R., Deloney L., Donepudi S., et. al.: Development and implementation of a systems-based practice project requirement for radiology residents. Acad Radiol 2008; 15: pp. 1040-1045.
34. Bohl M, Francois W, Gest T. 2011. Self-guided clinical cases for medical students based on postmortem CT scans of cadavers. Clin Anat 2011; 24:655–663.