Rationale and Objectives
To assess the American College of Radiology Incidental Findings Committee’s (ACR-IFC) recommendations for defining and following up abnormal incidental abdominopelvic lymph nodes.
Materials and Methods
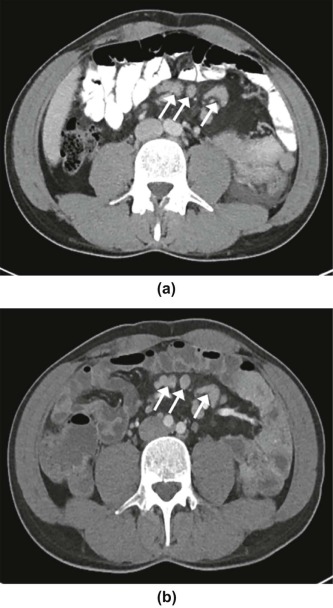
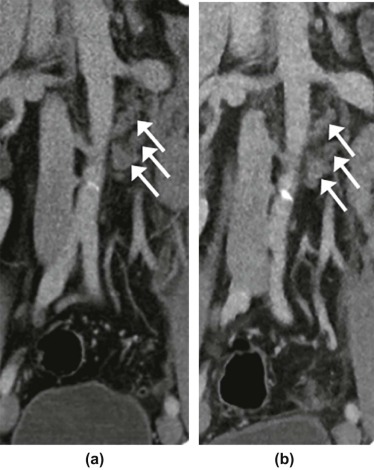
A total of 59 lymph nodes satisfying ACR-IFC criteria as incidental (no malignancy or lymphoproliferative disorder) and with sufficient follow-up to classify as benign (biopsy, decreased size, ≥12-month stability) or malignant (biopsy, detection of primary malignancy combined with either fluorodeoxyglucose hyperactivity or increase in size of the node) were included. Two radiologists independently assessed nodes for suspicious features by ACR-IFC criteria (round with indistinct hilum, hypervascularity, necrosis, cluster ≥3 nodes, cluster ≥2 nodes in ≥2 stations, size ≥1 cm in retroperitoneum). Outcomes were assessed with attention to ACR-IFC’s recommendation for initial 3-month follow-up.
Results
A total of 8.5% of nodes were malignant; 91.5% were benign. Two of six malignant nodes were stable at 3 to <6-month follow-up before diagnosis; diagnosis of four of five malignant nodes was facilitated by later development of non-nodal sites of tumor. A total of 13, 5, 8, and 9 nodes were deemed benign given a decrease at <3 months, 3–5 months, 6–11 months, or ≥12 months of follow-up. No ACR-IFC feature differentiated benign and malignant nodes ( P = 0.164–1.0). A cluster ≥3 nodes was present in 88.1%–93.2% of nodes. A total of 96.6%–98.3% had ≥1 suspicious feature for both readers. Necrosis and hypervascularity were not identified in any node.
Conclusions
ACR-IFC imaging features overwhelmingly classified incidental nodes as abnormal, although did not differentiate benign and malignant nodes. Nodes stable at the ACR-IFC’s advised initial 3-month follow-up were occasionally proven malignant or decreased on further imaging. Refinement of imaging criteria to define nodes of particularly high risk, integrated with other clinical criteria, may help optimize the follow-up of incidental abdominopelvic lymph nodes.
Introduction
Incidental lymph nodes are a common finding on abdominopelvic imaging, although are benign in a large majority of cases , rarely representing malignancy. However, benign and malignant lymph nodes overlap in imaging features as well as in their behavior on initial short-term follow-up imaging . Given their frequency and nonspecific imaging characteristics, incidental lymph nodes present a large diagnostic challenge that may ultimately be associated with clinical uncertainty, patient anxiety, and excess follow-up imaging.
To address this challenge, the American College of Radiology Incidental Findings Committee (ACR-IFC) published a white paper in 2013 addressing the management of incidental abdominopelvic lymph nodes on computed tomography (CT) . This white paper sought to provide both imaging criteria for considering nodes to be abnormal and warranting further evaluation, as well as guidance regarding the appropriate imaging surveillance of such nodes. According to the ACR-IFC, incidental lymph nodes are deemed abnormal if showing at least one of any of a set of imaging features incorporating nodal number, size, architecture, and enhancement pattern. For nodes deemed to be abnormal, the white paper emphasizes the value of a comparison to any relevant prior imaging. For patients with a known or suspected malignancy or lymphoproliferative disorder, further evaluation of the node, including possible biopsy, is suggested at the time of detection, as clinically appropriate. For incidental nodes in remaining patients, a short-term follow-up CT is suggested in approximately 3 months to allow time for interval clinical management and response to any intervening antibiotics or other medical management. This short-term 3-month examination similarly applies for follow-up of lymph nodes in patients with non-neoplastic conditions, such as acute pancreatitis, to assess for improvement or resolution. Furthermore, incidental lymph nodes may be deemed benign and not warranting any further imaging or other evaluation if remaining stable on follow-up imaging after 1 year.
Get Radiology Tree app to read full this article<
Methods
Patients
Get Radiology Tree app to read full this article<
Image and Clinical Evaluation
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Assessment
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
TABLE 1
Summary of Malignant Lymph Nodes
Node Location Maximal Short-Axis Size (mm) Diagnosis Reference Standard Reason Nodal Biopsy Was Performed Node Behavior on Follow-Up Imaging Before Diagnosis Mesenteric 7 B-cell lymphoma Nodal biopsy Patient with celiac disease; persistent abnormal nodes on follow-up imaging; interval endoscopy concerning for bowel malignancy Stable
at 4 months Perigastric 13 Mantle cell lymphoma Subsequently diagnosed primary malignancy and increased size of node on follow-up imaging n/a (no nodal biopsy performed) Increased
at 8 months Retroperitoneal, iliac chain 11 Lung cancer metastasis Subsequently diagnosed primary malignancy and node showing increased FDG activity on PET n/a (no nodal biopsy performed) Stable
at 1 month Mesenteric 19 Small bowel adenocarcinoma metastasis Nodal biopsy Follow-up imaging demonstrating a primary tumor not initially detected; interval increased size of node on follow-up imaging Increased
at 8 months Mesenteric, retroperitoneal, iliac chain 13 Low-grade follicular lymphoma Nodal biopsy Persistent widespread nodal enlargement on follow-up imaging Stable
at 5 month
FDG, fluorodeoxyglucose; PET, positron emission tomography.
TABLE 2
Summary of Benign Lymph Nodes, Based on Criteria for Deeming Nodes Benign
Benign Nodes Frequency, Benign Biopsy \* 9.4% (5 of 54) Decrease in size 68.5% (37 of 54) Decreased at <3 months 24.1% (13 of 54) Decreased at 3 to <6 months 9.3% (5 of 54) Decreased at 6 to <12 months (one stable at 3 to <6months; the remainder with no 3 to 6-month imaging) 16.7% (9 of 54) Decreased at >12 months (one stable at 6–12 months; the remainder with no 3 to 12-month imaging) 18.5% (10 of 54) Stable size at ≥12 months 25.9% (14 of 54) Stable at ≥24 months5.6% (3 of 54)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 3
Frequency and Inter-Reader Agreement of Abnormal Features at Subjective Analysis
Feature Reader 1 Reader 2 Concordant
Reading Kappa Abnormal architecture
(round, indistinct hilum) 81.4%(48of59) 72.9%(43of59) 74.6%(44of59) 0.320 Necrosis 0%(0of59) 0%(0of59) 100%(59of59) — Hypervascularity 0%(0of59) 0%(0of59) 100%(59of59) — Cluster of ≥3 nodes in one station 93.2%(55of59) 88.1%(52of59) 94.9%(56of59) 0.586 Cluster of ≥2 nodes in ≥2 stations 57.6%(34of59) 49.2%(29of59) 88.1%(52of59) 0.784 ≥1 abnormal subjective feature 98.3%(58of59) 96.6%(57of59) 98.3%(58of59) 0.488
TABLE 4
Comparison of Frequency of Abnormal Findings Between Benign and Malignant Nodes
Reader Features Benign Malignant_P_ 1 Architecture 79.6%(43of54) 100.0%(5of5) 0.573 1 Cluster of ≥3 nodes in one station 94.4%(51of54) 80.0%(4of5) 0.305 1 Cluster of ≥2 nodes in ≥2 stations 57.4%(31of54) 60.0%(3of5) 1.0 1 Any subjective feature 98.1%(53of54) 100%(5of5) 1.0 2 Architecture 74.1%(40of54) 60.0%(3of5) 0.606 2 Cluster of ≥3 nodes in one station 88.9%(48of54) 80.0%(4of5) 0.481 2 Cluster of ≥2 nodes in ≥2 stations 50.0%(27of54) 40.0%(2of5) 1.0 2 Any subjective feature 98.1%(53of54) 80.0%(4of5) 0.164 Either Any subjective feature 98.1%(53of54) 100%(5of5) 1.0 n/a Size 20.4%(11of54) 40.0%(2of5) 0.303 Either Any subjective feature or size 100%(54of54) 100.0%(5of5) 1.0
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Lumbreras B., Donat L., Hernandez-Aguado I.: Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol 2010; 83: pp. 276-289.
2. Lucey B.C., Stuhlfaut J.W., Soto J.A.: Mesenteric lymph nodes seen at imaging: causes and significance. Radiographics 2005; 25: pp. 351-365.
3. Matsuoka H., Masaki T., Sugiyama M., et. al.: Morphological characteristics of lateral pelvic lymph nodes in rectal carcinoma. Langenbecks Arch Surg 2007; 392: pp. 543-547.
4. Grubnic S., Vinnicombe S.J., Norman A.R., et. al.: MR evaluation of normal retroperitoneal and pelvic lymph nodes. Clin Radiol 2002; 57: pp. 193-200. discussion 201-194
5. Stigt J.A., Boers J.E., Oostdijk A.H., et. al.: Mediastinal incidentalomas. J Thorac Oncol 2011; 6: pp. 1345-1349.
6. Heller M.T., Harisinghani M., Neitlich J.D., et. al.: Managing incidental findings on abdominal and pelvic CT and MRI, part 3: white paper of the ACR Incidental Findings Committee II on splenic and nodal findings. J Am Coll Radiol 2013; 10: pp. 833-839.
7. Berland L.L.: Overview of white papers of the ACR Incidental Findings Committee II on adnexal, vascular, splenic, nodal, gallbladder, and biliary findings. J Am Coll Radiol 2013; 10: pp. 672-674.
8. Davenport M.S., Khalatbari S., Liu P.S., et. al.: Repeatability of diagnostic features and scoring systems for hepatocellular carcinoma by using MR imaging. Radiology 2014; 272: pp. 132-142.
9. Arita T., Matsumoto T., Kuramitsu T., et. al.: Is it possible to differentiate malignant mediastinal nodes from benign nodes by size? Reevaluation by CT, transesophageal echocardiography, and nodal specimen. Chest 1996; 110: pp. 1004-1008.
10. Markl B., Rossle J., Arnholdt H.M., et. al.: The clinical significance of lymph node size in colon cancer. Mod Pathol 2012; 25: pp. 1413-1422.
11. Dorfman R.E., Alpern M.B., Gross B.H., et. al.: Upper abdominal lymph nodes: criteria for normal size determined with CT. Radiology 1991; 180: pp. 319-322.
12. Eisenhauer E.A., Therasse P., Bogaerts J., et. al.: New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009; 45: pp. 228-247.
13. Baxa J., Vondrakova A., Matouskova T., et. al.: Dual-phase dual-energy CT in patients with lung cancer: assessment of the additional value of iodine quantification in lymph node therapy response. Eur Radiol 2014; 24: pp. 1981-1988.
14. Yasui O., Sato M., Kamada A.: Diffusion-weighted imaging in the detection of lymph node metastasis in colorectal cancer. Tohoku J Exp Med 2009; 218: pp. 177-183.