We developed a longitudinal care coordination service to proactively deliver high-quality and family-centered care in patients receiving radioiodine therapy for thyroid cancer. In an iterative, multidisciplinary team manner, a pretherapy consultation service, which included scripted interactions, documentation, and checklists for quality control, evolved over time into a robust patient-centered longitudinal care coordination nuclear medicine service. Radiation safety precautions, the rationale for therapy, and management of patient expectations were addressed through the initial consultation, and discharge and posttreatment care were managed during subsequent follow-up. The patient–physician relationship created during longitudinal nuclear medicine therapy care is one tool to help counteract the growing commoditization of radiology. This article describes the process that the nuclear medicine specialists in our department established to enhance radiologist value by providing both exceptional thyroid cancer treatment and continuity of care.
Given threats of commoditization and irrelevancy , the importance of patients identifying radiologists as full members of the health care team is clearer than ever . Opportunities abound for radiologists and nuclear medicine physicians to proactively deliver patient care in the same robust and personalized manner as many traditional clinical specialists. One of those areas is nuclear medicine therapeutics . Although therapeutic nuclear medicine interventions comprise a small proportion of the daily workload of most radiology practices, the opportunities for added value in the form of direct patient–physician relationships are disproportionately great.
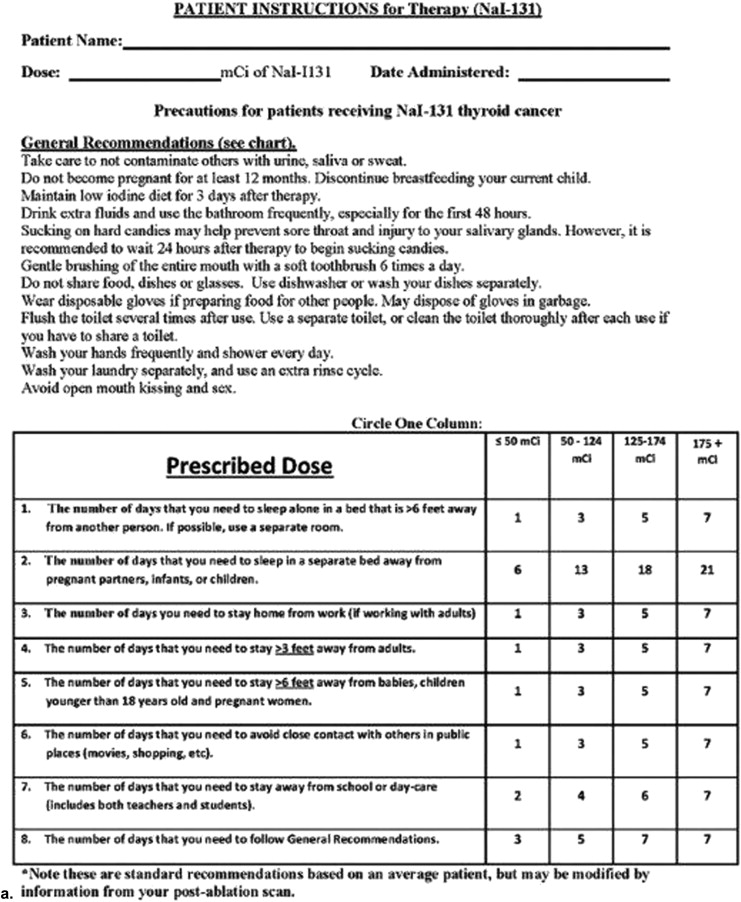
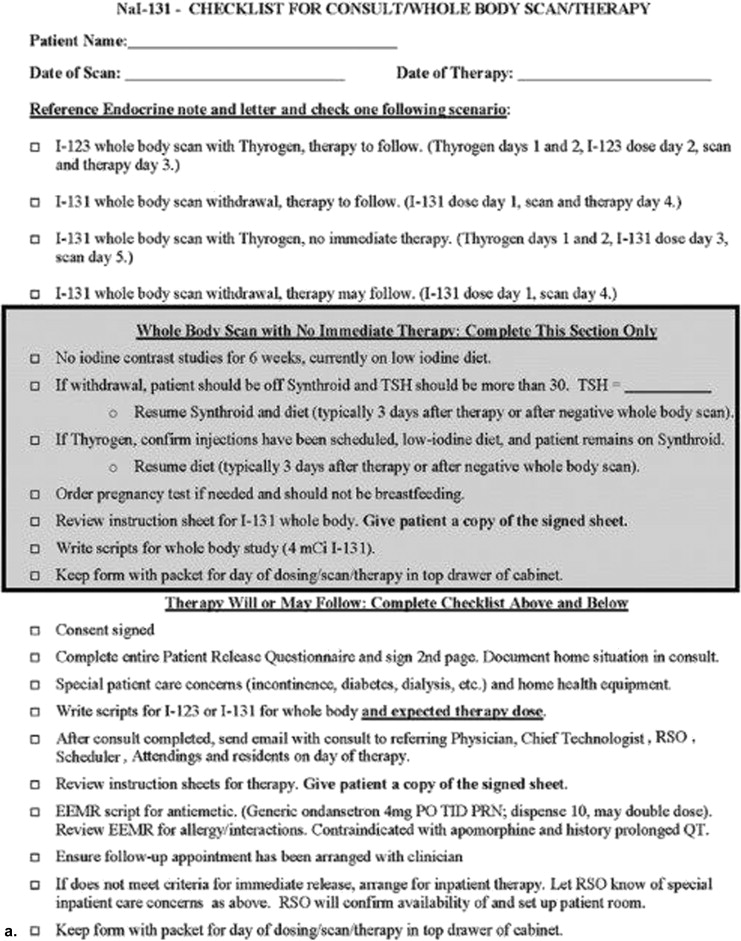
Modern nuclear medicine therapeutics encompasses a wide variety of molecular and anatomic targets. Although NaI-I-131 for thyroid cancer and hyperthyroidism is the oldest and most commonly used, all involve complex shared decision making with patients and referring physicians to address unique radiation safety precautions, patient preparation, and guideline adherence . Establishing a formal nuclear medicine physician–patient relationship before therapy allows practices to offer patient- and family-focused high-quality care while simultaneously improving institutional workflow efficiencies.
In this article, we outline our own experience establishing and refining a nuclear medicine therapy care coordination service for patients with thyroid carcinoma and focus on 1) improving communication and standardizing patient care by optimizing opportunities for patient contact and communication; 2) placing radiologists and nuclear medicine physicians in a central and active (rather than peripheral and passive) role in patient care; and 3) creating a vehicle to introduce improved quality control tools and organizing physicians and staff to participate in practice quality improvement (PQI) projects. The work described in this article represents a predominantly qualitative pilot project that was conceived as a quality improvement initiative.
The care coordination imperative
At our institution, like most, radioiodine thyroid cancer therapies were historically carried out as inpatient procedures after withdrawal of thyroid hormone replacement , and the nuclear medicine physician’s role was relegated to deciding the proper dose of radioiodine, rather than that of a consultant central to medical decision making. In some instances, the patient might actually meet the nuclear medicine practitioner for the first time at the time of dose administration.
In 2003, the Nuclear Regulatory Commission began to permit the delivery of high-dose radioiodine therapy in the outpatient setting , and in 2007, the FDA approved recombinant human thyroid-stimulating hormone, obviating the need for pretreatment thyroid hormone withdrawal and its associated side effects . These two advances created opportunities for improved care but also demanded a higher degree of coordination with referring providers, more sophisticated scheduling, and more complex patient preparation.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
The first iteration: the consult service
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Early program evaluation and PQI
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
The final product: the care coordination service
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Current experience
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Glazer G.M., Ruiz-Wibbelsmann J.A.: The invisible radiologist. Radiology 2011; 258: pp. 18-22.
2. Gilmore W.M.: The radiologist as a consultant. Can Med Assoc J 1940; 42: pp. 357-360.
3. Grant L., Griffin N., McDonald S., et. al.: The role of a consultant radiologist—are patients still in the dark?. Eur Radiol 2009; 19: pp. 2326-2332.
4. Kaufman S.A.: Radiologist as consultant. AJR Am J Roentgenol 1979; 133: pp. 162-163.
5. Kessler H.B.: The contemporary radiologist: consultant or film reader?. AJR Am J Roentgenol 1997; 169: pp. 353-354.
6. Koo P.J., Bagrosky B.M.: Nuclear medicine therapy clinics: a golden opportunity for direct longitudinal patient care. J Am Coll Radiol 2014; 11: pp. 219-220.
7. Rogers L.F., Potchen E.J., Maynard C.D.: The radiologist as a primary care extender. Radiology 1995; 194: pp. 19-22.
8. Bodei L., Mueller-Brand J., Baum R.P., et. al.: The joint IAEA, EANM, and SNMMI practical guidance on peptide receptor radionuclide therapy (PRRNT) in neuroendocrine tumours. Eur J Nucl Med Mol Imaging 2013; 40: pp. 800-816.
9. Sisson J.C., Freitas J., McDougall I.R., et. al.: Radiation safety in the treatment of patients with thyroid diseases by radioiodine 131I: practice recommendations of the American Thyroid Association. Thyroid 2011; 21: pp. 335-346.
10. Silberstein E.B., Alavi A., Balon H.R., et. al.: The SNMMI practice guideline for therapy of thyroid disease with 131I 3.0. J Nucl Med 2012; 53: pp. 1633-1651.
11. Grigsby P.W., Siegel B.A., Baker S., et. al.: Radiation exposure from outpatient radioactive iodine (131I) therapy for thyroid carcinoma. JAMA 2000; 283: pp. 2272-2274.
12. United States Nuclear Regulatory Commission. NRC: FSME - NRC SECY 96–100: “Final Amendments to 10 CFR Parts 20 and 35 on Criteria for the Release of Individuals”. Accessed on January 14, 2014.
13. Willegaignon J., Sapienza M., Ono C., et. al.: Outpatient radioiodine therapy for thyroid cancer: a safe nuclear medicine procedure. Clin Nucl Med 2011; 36: pp. 440-445.
14. 2012.Genzyme CorporationCambridge, MA
15. Haugen B.R., Cooper D.S., Emerson C.H., et. al.: Expanding indications for recombinant human TSH in thyroid cancer. Thyroid 2008; 18: pp. 687-694.
16. Haugen B.R., Pacini F., Reiners C., et. al.: A comparison of recombinant human thyrotropin and thyroid hormone withdrawal for the detection of thyroid remnant or cancer. J Clin Endocrinol Metab 1999; 84: pp. 3877-3885.
17. Ginsberg L.E.: Radiologists as physicians. Radiology 2009; 250: pp. 605-606.
18. Gunderman R.B.: The medical community’s changing vision of the patient: the importance of radiology. Radiology 2005; 234: pp. 339-342.
19. Maynard C.D.: Radiologists: physicians or expert image interpreters?. Radiology 2008; 248: pp. 333-336.
20. Mettler F.A., Guiberteau M.J.: Essentials of nuclear medicine imaging.6th ed.2012.Elsevier/SaundersPhiladelphia, PA
21. Cooper D.S., Doherty G.M., Haugen B.R., et. al.: Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009; 19: pp. 1167-1214.
22. Salama J.K., Golden D.W., Yom S.S., et. al.: ACR Appropriateness Criteria (R) thyroid carcinoma. Oral Oncol 2014; 50: pp. 577-586.
23. Hales B., Terblanche M., Fowler R., et. al.: Development of medical checklists for improved quality of patient care. Int J Qual Health Care 2008; 20: pp. 22-30.
24. Hales B.M., Pronovost P.J.: The checklist—a tool for error management and performance improvement. J Crit Care 2006; 21: pp. 231-235.
25. ACR: Nuclear Medicine Coding User Guides.2014.
26. Forman H.P., Larson D.B., Kaye A.D., et. al.: Masters of radiology panel discussion: the commoditization of radiology. AJR Am J Roentgenol 2011; 196: pp. 843-847.
27. Afable R., Brant-Zawadzki M.N.: Changing radiology in the changing hospital environment. J Am Coll Radiol 2013; 10: pp. 887-889.