Rationale and Objectives
Development of imaging biomarkers often relies on their correlation with histopathology. Our aim was to compare two approaches for correlating pathology to multiparametric magnetic resonance (MR) imaging (mpMRI) for localization and quantitative assessment of prostate cancer (PCa) index tumor using whole mount (WM) pathology (WMP) as the reference.
Materials and Methods
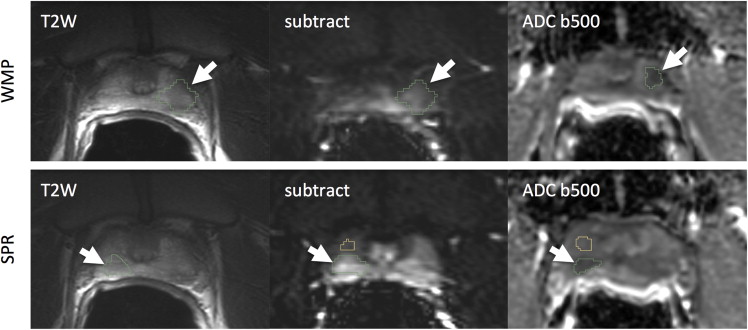
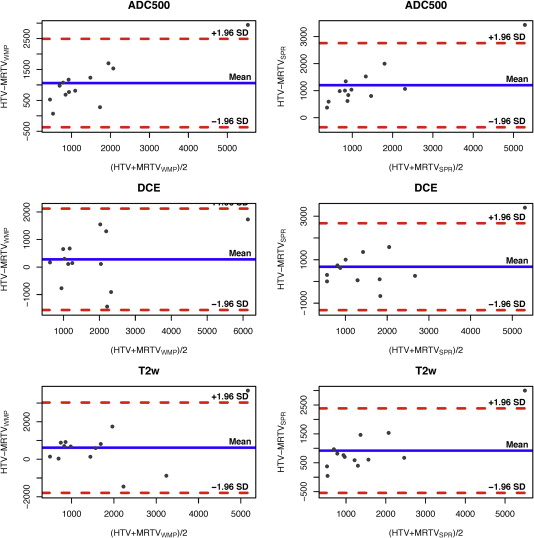
Patients ( N = 30) underwent mpMRI that included diffusion-weighted imaging and dynamic contrast-enhanced (DCE) MRI at 3 T before radical prostatectomy (RP). RP specimens were processed using WM technique (WMP) and findings summarized in a standard surgical pathology report (SPR). Histology index tumor volumes (HTVs) were compared to MR tumor volumes (MRTVs) using two approaches for index lesion identification on mpMRI using annotated WMP slides as the reference (WMP) and using routine SPR as the reference. Consistency of index tumor localization, tumor volume, and mean values of the derived quantitative parameters (mean apparent diffusion coefficient [ADC], K trans , and v e ) were compared.
Results
Index lesions from 16 of 30 patients met the selection criteria. There was WMP/SRP agreement in index tumor in 13 of 16 patients. ADC-based MRTVs were larger ( P < .05) than DCE-based MRTVs. ADC MRTVs were smaller than HTV ( P < .005). There was a strong correlation between HTV and MRTV (Pearson ρ > 0.8; P < .05). No significant differences were observed in the mean values of K trans and ADC between the WMP and SPR.
Conclusions
WMP correlation is superior to SPR for accurate localization of all index lesions. The use of WMP is however not required to distinguish significant differences of mean values of quantitative MRI parameters within tumor volume.
Magnetic resonance (MR) imaging (MRI) of the prostate has become an essential modality for staging and characterizing prostate cancer (PCa) . Current imaging protocols use multiparametric MRI (mpMRI) with diffusion-weighted imaging (DWI) and dynamic contrast-enhanced (DCE) MRI in addition to conventional T2- and T1-weighted imaging for a comprehensive assessment of PCa. The current recommendations for the clinical use of MRI rely on the qualitative assessment of the MR parameters , but much work is currently being done to refine mpMRI acquisitions, analyses, and validations to establish the clinical utility of quantitative prostate imaging. Each individual imaging sequence can provide unique and complementary quantitative measurements of the underlying physiology and pathophysiology of the prostate tissue, leading to improved detection of PCa . However, exactly what pathophysiology these quantitative measurements represent is not well established.
Development and validation of quantitative imaging tools requires correlation with established markers of the disease. A pathology-derived Gleason score remains the cornerstone for decision making with regard to therapy selection and disease prognosis . As such, numerous studies have been conducted to correlate quantitative mpMRI parameters with histology for the purposes of localizing the lesion and assessing its aggressiveness . Likewise, correlation with histology is also a necessary component in the validation of mpMRI as a means of response to therapy. However, the methods used for pathologic correlation vary widely, ranging from in-depth whole mount (WM) processing of the specimen followed by delineation of tumor foci by a pathologist directly on the glass sides and comparison to MRI data, to simply correlating MR images to the standard clinical pathology report. These two correlative pathology approaches are very different in terms of resources, expertise, and time involvement. WM pathology (WMP) correlation requires a technologist with expertise in WM fixation, embedding and sectioning, extensive pathologist involvement and is considered the “gold standard” for an imaging correlative approach. In contrast to standard pathologic processing used routinely, where individual cross-sections of the prostate are further cut into four quadrants or more, WMP allows for increased accuracy of the spatial mapping between pathology specimen and images, as axial sections of the prostate specimen are processed using large WM slides, which are marked to facilitate volumetric reconstruction of the specimen. The tumor areas are next contoured on each slide, thus simplifying spatial localization of the matching lesions in the imaging data. This in-depth correlative approach has been used by many . In contrast, a more common routine processing protocol provides pathology information necessary for clinical decision making, and including overall Gleason score and whether or not there is an extracapsular extension of tumor, it may include one- or two-dimensional measurement of the tumor area(s). As such, routine processing does not allow for volumetric reconstruction of the specimen, and so, three-dimensional volumes cannot be easily estimated. The surgical pathology report (SPR) is therefore not focused on providing detailed information for validating imaging studies. However, given the ubiquitous availability of SPR data, and the relatively low cost of implementing imaging correlative studies that rely on SPR, the practical question is whether SPR alone is sufficient for accurate localization of PCa. If the index lesion is correctly localized, it is unknown whether the assumed improvement in the accuracy of tumor delineation using WMP leads to significant differences in the tumor volume outlined, or differences in the quantitative MR parameters obtained.
Get Radiology Tree app to read full this article<
Materials and methods
Patients
Get Radiology Tree app to read full this article<
MR Imaging
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Image Processing
Get Radiology Tree app to read full this article<
Histopathology Acquisition and Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Lesion Localization
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Comparison Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Study Population
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Comparative Analysis between Pathologic Approaches
Index Lesion Localization
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Tumor Volume Assessment
Get Radiology Tree app to read full this article<
Table 1
Tumor Volume Estimates From the Individual MRI Sequences Using SPR and WMP Correlative Approaches (MRTV SPR and MRTV WMP , Respectively) and Their Differences Versus HTV
mpMRI Parameter Mean (SD) MRTV SPR , mm 3 Mean (SD) Difference between HTV and MRTV SPR , mm 3 Mean (SD) MRTV WMP , mm 3 Mean (SD) Difference between HTV and MRTV WMP , mm 3 T2WI 1073 (1022)* 919 (745) 1376 (1176) 626 (1229) DCE 1314 (974) 678 (1021) 1711 (1303) 280 (940) ADC 790 (950)* 1202 (794) 931 (1036)* 1061 (730)
ADC, apparent diffusion coefficient; DCE, dynamic contrast enhanced; HTV, histology index tumor volume; mpMRI, multiparametric magnetic resonance imaging; MRI, magnetic resonance imaging; MRTV, magnetic resonance tumor volumes; SD, standard deviation; SPR, surgical pathology report; T2WI, T2-weighted imaging; WMP, whole mount pathology.
MRI-based measurements that were significantly smaller ( P < .005) than HTV based on three-way pairwise comparison between the SPR, WMP, and HTV measurements are marked with asterisk.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Comparison of Quantitative Multiparametric Parameters between Tumor and Nontumor ROIs
Get Radiology Tree app to read full this article<
Table 2
Mean Quantitative Parameters Extracted From the Tumor and Normal ROI Delineated Using WMP and SPR Approaches
mpMRI Parameter SPR, Tumor SPR, Normal WMP, Tumor WMP, Normal K trans , min −1 0.4 (0.17) 0.19 (0.1) 0.37 (0.13) 0.18 (0.09) v e 0.26 (0.07) 0.2 (0.1) 0.26 (0.08) 0.2 (0.05) ADC b500, × 10 −6 mm 2 /s 978 (200) 1714 (237) 1018 (181) 1542 (160)
ADC, apparent diffusion coefficient; mpMRI, multiparametric magnetic resonance imaging; ROI, region of interest; SPR, surgical pathology report; WMP, whole mount pathology.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Summary of the Advantages and Disadvantages between the WMP and SPR-based Pathology to Imaging Correlation Methods
Imaging to Pathology Correlation Approach Advantages Disadvantages Whole mount processing (WMP)
Surgical pathology report (SPR)
SPR, surgical pathology report; WMP, whole mount pathology.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgments
Get Radiology Tree app to read full this article<
References
1. Hegde J.V., Mulkern R.V., Panych L.P., et. al.: Multiparametric MRI of prostate cancer: an update on state-of-the-art techniques and their performance in detecting and localizing prostate cancer. J Magn Reson Imaging 2013; 37: pp. 1035-1054.
2. Dickinson L., Ahmed H.U., Allen C., et. al.: Magnetic resonance imaging for the detection, localisation, and characterisation of prostate cancer: recommendations from a European consensus meeting. Eur Urol 2011; 59: pp. 477-494.
3. Barentsz J.O., Richenberg J., Clements R., et. al.: ESUR prostate MR guidelines 2012. Eur Radiol 2012; 22: pp. 746-757.
4. Stamatakis L., Siddiqui M.M., Nix J.W., et. al.: Accuracy of multiparametric magnetic resonance imaging in confirming eligibility for active surveillance for men with prostate cancer. Cancer 2013; pp. 1-8.
5. Arumainayagam N., Ahmed H.U., Moore C.M., et. al.: Multiparametric MR imaging for detection of clinically significant prostate cancer: a validation cohort study with transperineal template prostate mapping as the reference standard. Radiology 2013; 268: pp. 761-769.
6. Heidenreich A., Bellmunt J., Bolla M., et. al.: EAU guidelines on prostate cancer. Part I: screening, diagnosis, and treatment of clinically localised disease. Eur Urol 2011; 59: pp. 61-71.
7. Turkbey B., Mani H., Shah V., et. al.: Multiparametric 3T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol 2011; 186: pp. 1818-1824.
8. Langer D.L., van der Kwast T.H., Evans A.J., et. al.: Prostate tissue composition and MR measurements: investigating the relationships between ADC, T2, K(trans), v(e), and corresponding histologic features. Radiology 2010; 255: pp. 485-494.
9. Turkbey B., Mani H., Aras O., et. al.: Correlation of magnetic resonance imaging tumor volume with histopathology. J Urol 2012; 188: pp. 1157-1163.
10. Mazaheri Y., Hricak H., Fine S.W., et. al.: Prostate tumor volume measurement with combined T2-weighted imaging and diffusion-weighted MR: correlation with pathologic tumor volume. Radiology 2009; 252: pp. 449-457.
11. Fennessy F.M., Fedorov A., Gupta S.N., et. al.: Practical considerations in T1 mapping of prostate for dynamic contrast enhancement pharmacokinetic analyses. Magn Reson Imaging 2012; 30: pp. 1224-1233.
12. Tofts P.S., Brix G., Buckley D.L., et. al.: Estimating kinetic parameters from contrast-enhanced T1-weighted MRI of a diffusable tracer: standardized quantities and symbols. J Magn Reson Imaging 1999; 10: pp. 223-232.
13. De Bazelaire C.M.J., Duhamel G.D., Rofsky N.M., et. al.: MR imaging relaxation times of abdominal and pelvic tissues measured in vivo at 3.0 T: preliminary results. Radiology 2004; 230: pp. 652-659.
14. Carr J.C., Carroll T.J.: Magnetic resonance angiography: principles and applications.2011.Springer
15. Fritz-Hansen T., Rostrup E., Larsson H.B., et. al.: Measurement of the arterial concentration of Gd-DTPA using MRI: a step toward quantitative perfusion imaging. Magn Reson Med 1996; 36: pp. 225-231.
16. Weinmann H.J., Laniado M., Mützel W.: Pharmacokinetics of GdDTPA/dimeglumine after intravenous injection into healthy volunteers. Physiol Chem Phys Med NMR 1984; 16: pp. 167-172.
17. Priest A.N., Gill A.B., Kataoka M., et. al.: Dynamic contrast-enhanced MRI in ovarian cancer: initial experience at 3 tesla in primary and metastatic disease. Magn Reson Med 2010; 63: pp. 1044-1049.
18. Trivedi H., Turkbey B., Rastinehad A.R., et. al.: Use of patient-specific MRI-based prostate mold for validation of multiparametric MRI in localization of prostate cancer. Urology 2012; 79: pp. 233-239.
19. Fedorov A., Beichel R., Kalpathy-Cramer J., et. al.: 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn Reson Imaging 2012; 30: pp. 1323-1341.
20. Jonmarker S., Valdman A., Lindberg A., et. al.: Tissue shrinkage after fixation with formalin injection of prostatectomy specimens. Virchows Arch 2006; 449: pp. 297-301.
21. Wolters T., Roobol M.J., van Leeuwen P.J., et. al.: A critical analysis of the tumor volume threshold for clinically insignificant prostate cancer using a data set of a randomized screening trial. J Urol 2011; 185: pp. 121-125.
22. Stamey T.A., Freiha F.S., McNeal J.E., et. al.: Localized prostate cancer. Relationship of tumor volume to clinical significance for treatment of prostate cancer. Cancer 1993; 71: pp. 933-938.
23. Zou K.H., Warfield S.K., Bharatha A., et. al.: Statistical validation of image segmentation quality based on a spatial overlap index. Acad Radiol 2004; 11: pp. 178-189.
24. Wang L., Mazaheri Y., Zhang J., et. al.: Assessment of biologic aggressiveness of prostate cancer: correlation of MR signal intensity with Gleason grade after radical prostatectomy. Radiology 2008; 246: pp. 168-176.
25. Wang X.Z., Wang B., Gao Z.Q., et. al.: Diffusion-weighted imaging of prostate cancer: correlation between apparent diffusion coefficient values and tumor proliferation. J Magn Reson Imaging 2009; 29: pp. 1360-1366.
26. Zelhof B., Lowry M., Rodrigues G., et. al.: Description of magnetic resonance imaging-derived enhancement variables in pathologically confirmed prostate cancer and normal peripheral zone regions. BJU Int 2009; 104: pp. 621-627.
27. Ren J., Huan Y., Wang H., et. al.: Dynamic contrast-enhanced MRI of benign prostatic hyperplasia and prostatic carcinoma: correlation with angiogenesis. Clin Radiol 2008; 63: pp. 153-159.
28. Rud E., Klotz D., Rennesund K., et. al.: Detection of the index tumor and tumor volume in prostate cancer using T2W and DW MRI alone. BJU Int 2014; 114: pp. E32-E42.
29. Le Nobin J., Orczyk C., Deng F.-M., et. al.: Prostate tumor volumes: agreement between MRI and histology using novel co-registration software. BJU Int 2014; 114: pp. E105-E112.
30. Cornud F., Khoury G., Bouazza N., et. al.: Tumor target volume for focal therapy of prostate cancer-does multiparametric magnetic resonance imaging allow for a reliable estimation?. J Urol 2014; 191: pp. 1272-1279.
31. Ward A.D., Crukley C., McKenzie C.A., et. al.: Prostate: registration of digital histopathologic images to in vivo MR images acquired by using endorectal receive coil. Radiology 2012; 263: pp. 856-864.
32. Meyer C., Ma B., Kunju L.P., et. al.: Challenges in accurate registration of 3-D medical imaging and histopathology in primary prostate cancer. Eur J Nucl Med Mol Imaging 2013; 40: pp. S72-S78.
33. Hollenbeck B.K., Bassily N., Wei J.T., et. al.: Whole mounted radical prostatectomy specimens do not increase detection of adverse pathological features. J Urol 2000; 164: pp. 1583-1586.
34. Noguchi M., Stamey T.A., McNeal J.E., et. al.: Prognostic factors for multifocal prostate cancer in radical prostatectomy specimens: lack of significance of secondary cancers. J Urol 2003; 170: pp. 459-463.
35. Wise A.M., Stamey T.A., McNeal J.E., et. al.: Morphologic and clinical significance of multifocal prostate cancers in radical prostatectomy specimens. Urology 2002; 60: pp. 264-269.
36. Kozlowski P., Chang S.D., Jones E.C., et. al.: Combined diffusion-weighted and dynamic contrast-enhanced MRI for prostate cancer diagnosis–correlation with biopsy and histopathology. J Magn Reson Imaging 2006; 24: pp. 108-113.
37. Epstein J.I., Walsh P.C., Sauvageot J., et. al.: Use of repeat sextant and transition zone biopsies for assessing extent of prostate cancer. J Urol 1997; 158: pp. 1886-1890.
38. Stroumbakis N., Cookson M.S., Reuter V.E., et. al.: Clinical significance of repeat sextant biopsies in prostate cancer patients. Urology 1997; 49: pp. 113-118.
39. Svetec D., McCabe K., Peretsman S., et. al.: Prostate rebiopsy is a poor surrogate of treatment efficacy in localized prostate cancer. J Urol 1998; 159: pp. 1606-1608.