Rationale and Objectives
With advancements in technology and push for health care reform and reduced costs, minimally invasive procedures, such as those that are ultrasound-guided, have become an essential part of radiology, and are used in many divisions of radiology. By incorporating standardized training methodologies in a risk free environment through utilization of a simulation center with phantom training, we hope to improve proficiency and confidence in procedural performance.
Materials and Methods
Twenty-nine radiology residents from four levels of training were enrolled in this prospective study. The residents were given written, video, and live interactive training on the basics of ultrasound-guided procedures in our simulation center on a phantom mannequin. All of the teaching materials were created by residents and staff radiologists at the institution.
Results
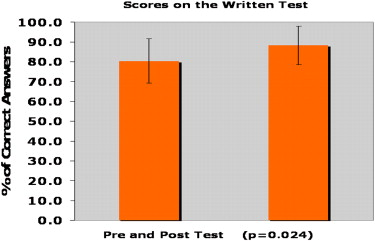
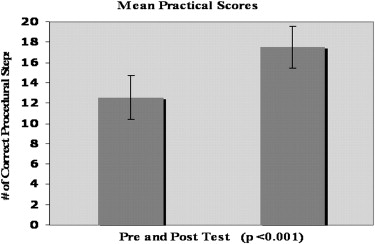
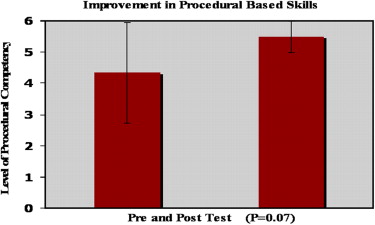
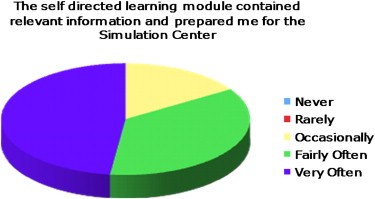
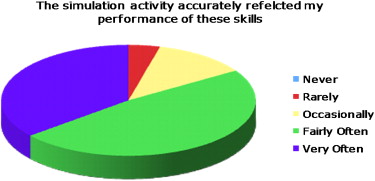
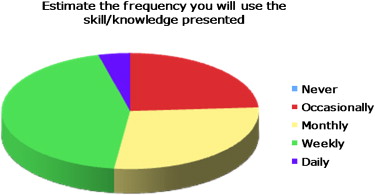
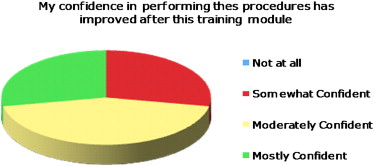
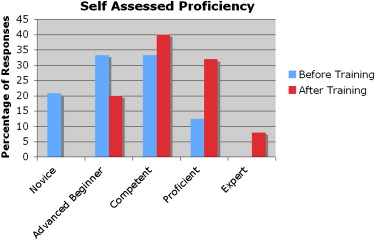
Residents demonstrated statistically significant improvement ( P < .05) between their pre- and posttest scores on both the written and practical examinations. They also showed a trend toward improved dexterity in the technical aspects of ultrasound-guided procedures ( P = .07) after training. On the survey questionnaire, residents confirm improved knowledge level, technical ability, and confidence levels pertaining to ultrasound-guided procedures.
Conclusions
The use of controlled simulation based training can be an invaluable tool to improve the knowledge level, dexterity, and confidence of residents performing ultrasound-guided procedures. Additionally, a simulation model allows standardization of education.
The modifications in health care over the past few decades have changed the face of medical education training. Federal restrictions have mandated strict duty hours compliance and an emphasis on shorter inpatient hospital stays, which translates into fewer training opportunities to perform and become proficient at minimally invasive procedures , changes which may affect patient care and safety issues. Because of these adjustments, the time-honored traditional model of medical education, which uses an apprenticeship approach to training, may need to be reevaluated and augmented with additional training. The traditional model of medical education, also known as the Halstedian model of education , uses patients as tools for teaching, with residents gaining an increased level of independence and responsibility through progression of training, under the supervision of faculty . A proficiency-based model of training may be a useful adjuvant to augment training. An example of proficiency-based training is the use of simulation, which allows a medical procedure to be learned based on a system of standard metrics, and hence progress can be recorded.
Performing an ultrasound-guided procedure is one of the basic aspects of a radiologist’s training, and is essential for many therapeutic and diagnostic procedures. Ultrasound-guided procedures are performed in many divisions of radiology including mammography, body imaging, interventional radiology, and musculoskeletal imaging. Targeted needle placement requires distinct psychomotor abilities and good hand-eye coordination . As previously mentioned, the apprenticeship approach to training of procedures has led to no existing standards of teaching or objectively rating the radiologists’ ability to safely practice these procedures . We propose the development and utilization of a simulation-based model in training residents to learn and become both proficient and confident in performing ultrasound-guided procedures by utilization of a web-based model and a physical phantom, in hope that this will ultimately translate to improved patient care and safety.
Materials and methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appendix A
Sample pretest and posttest questions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appendix B
Ultrasound-guided procedures checklist
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appendix C
Questions assessing the utility of simulator training for ultrasound-guided procedures
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Desser T.S.: Simulation-based training: the next revolution in radiology education?. J Am Coll Radiol 2007; 4: pp. 816-824.
2. Dawson S.: Procedural simulation: a primer. Radiology 2006; 241: pp. 17-25.
3. Long D.M.: Competency-based residency training: the next advance in graduate medical education. Acad Med 2000; 75: pp. 1178-1183.
4. Magee D., Zhu Y., Ratnalingam R., et. al.: An augmented reality simulator for ultrasound guided needle placement training. Med Biol Eng Comput 2007; 45: pp. 957-967.
5. Patel A.A., Gould D.A.: Simulators in interventional radiology training and evaluation: a paradigm shift is on the horizon. J Vasc Interv Radiol 2006; 17: pp. S163-S173.
6. Towbin A.J., Paterson B.E., Chang P.J.: Computer-based simulator for radiology: an educational tool. Radiographics 2008; 28: pp. 309-316.
7. Gordon J.A., Oriol N.E., Cooper J.B.: Bringing good teaching cases “to life”: a simulator-based medical education service. Acad Med 2004; 79: pp. 23-27.
8. Ganai S., Donroe J.A., St Louis M.R., et. al.: Virtual-reality training improves angled telescope skills in novice laparoscopists. Am J Surg 2007; 193: pp. 260-265.
9. Seymour N.E., Gallagher A.G., Roman S.A., et. al.: Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 2002; 236: pp. 458-463. discussion 463–464
10. Gallagher A.G., Satava R.M.: Virtual reality as a metric for the assessment of laparoscopic psychomotor skills. Learning curves and reliability measures. Surg Endosc 2002; 16: pp. 1746-1752.
11. Bloom M.B., Rawn C.L., salzberg A.D., et. al.: Virtual reality applied to procedural testing: the next era. Ann Surg 2003; 237: pp. 442-448.
12. Korndorffer J.R., Dunne J.B., Sierra R., et. al.: Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 2005; 201: pp. 23-29.
13. Erinjeri J.P., Bhalla S.: Redefining radiology education for first-year medical students: shifting from a passive to an active case-based approach. Acad Radiol 2006; 13: pp. 789-796.
14. Evans A.W., Aghabeigi B., Lesson R., et. al.: Are we really as good as we think we are?. Ann R Coll Surg Engl 2002; 84: pp. 54-56.