Rationale and Objectives
Basal lung opacities are frequently observed on supine chest x-ray (SCXR) of intensive care patients, causing insecurity among clinicians and radiologists. We sought to determine the diagnostic accuracy of SCXR for basal pneumonia.
Materials and Methods
We identified 172 patients who received both SCXR and computed tomography within 1 hour. Two readers examined the SCXR and rated findings in both basal zones according to the following scale: 0 = “no pneumonia,” 1 = “possible pneumonia,” 2 = “highly suspected pneumonia.” Computed tomography served as standard of reference. Sensitivity, specificity, and positive and negative predictive values (PPV/NPV) were calculated once pooling 0 and 1 as negative and once pooling 1 and 2 as positive finding.
Results
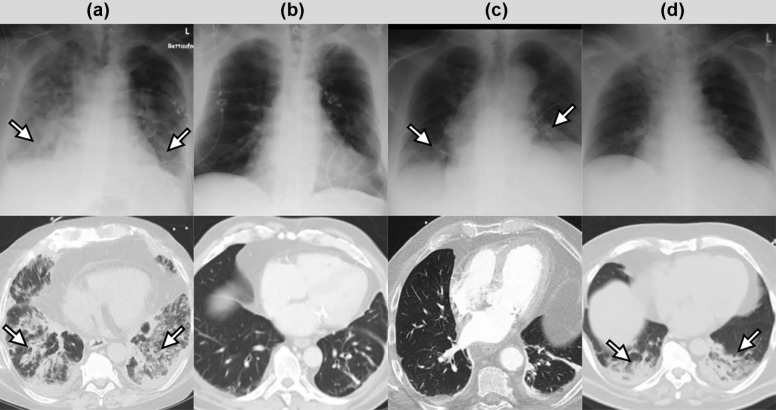
When pooling 0 and 1 as negative, sensitivity was 0.45 (right)/0.38 (left), specificity was 0.94/0.97, PPV was 0.76/0.79, and NPV was 0.81/0.84. When pooling 1 and 2 as positive, sensitivity was 0.80/0.75, specificity was 0.62/0.58, PPV was 0.45/0.35, and NPV was 0.88/0.89. The most common findings in false-positive cases were combined pleural effusions and lower lobe atelectasis.
Conclusions
Interpreting only highly suspicious basal opacities as pneumonia considerably increases the PPV with almost constant NPV. Clinicians and radiologists should be aware of the limitations of SCXR regarding basal pneumonia.
Introduction
Supine chest x-ray (SCXR) is the most commonly performed examination in modern intensive care medicine despite the technological advances in computed tomography (CT) imaging. Interpreting SCXR examinations still represents a diagnostic challenge. As daily routine use of SCXR provided no benefit regarding patient mortality and safety compared to an on-demand approach , several institutions have banned SCXR as a daily routine examination on intensive care units (ICUs).
Even in these institutions, SCXR remains a frequently performed diagnostic test in patients with suspected pulmonary infections. Importantly, pneumonia still prevails as the leading cause of death in ICU patients. Therefore, early and accurate diagnosis is a crucial task for intensive care physicians . Clinical and laboratory findings such as respiratory deterioration, raised inflammatory markers, fever, and sputum cultures can be very difficult to interpret in the context of the patients’ severe underlying diseases . Thus, imaging plays an important role in the diagnosis of pneumonia.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and Methods
Get Radiology Tree app to read full this article<
Patient Population
Get Radiology Tree app to read full this article<
Image Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
TABLE 1
Patient Characteristics
Patients_n_ = 172 Age—y \* 65.5 ± 14.2 Female sex—no. (%) 53 (30.8) CRP—mg/dL \* 9.2 ± 8.9 Underlying disease—no. (%) Vascular 50 (29) Infectious/Inflammatory 35 (20) Neoplastic 32 (19) Degenerative 8 (5) Iatrogenic 29 (17) Congenital 0 (0) Allergic/Autoimmune 1 (1) Traumatic 11 (6) Environmental/Exposure 6 (3)
CRP, C-reactive protein; ICU, intensive care unit.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 2
Diagnostic Accuracy of Supine Chest X-Ray Readings for Basal Pneumonia
SCXR Grading Rated as Positive Comparison to Previous Examination Patients No. Side Sensitivity Specificity PPV NPV 1 + 2 No 172 Right 0.80 (0.66–0.90) 0.62 (0.53–0.70) 0.45 (0.35–0.57) 0.88 (0.80–0.94) Left 0.75 (0.59–0.87) 0.58 (0.49–0.67) 0.35 (0.25–0.46) 0.89 (0.80–0.94) 1 + 2 Yes 124 Right 0.86 (0.70–0.95) 0.58 (0.48–0.69) 0.45 (0.33–0.57) 0.91 (0.81–0.97) Left 0.82 (0.63–0.94) 0.58 (0.48–0.68) 0.37 (0.25–0.50) 0.92 (0.82–0.97) 2 No 172 Right 0.45 (0.31–0.60) 0.94 (0.89–0.98) 0.76 (0.57–0.90) 0.81 (0.74–0.87) Left 0.38 (0.23–0.54) 0.97 (0.92–0.99) 0.79 (0.54–0.94) 0.84 (0.77–0.89) 2 Yes 124 Right 0.51 (0.34–0.69) 0.89 (0.80–0.95) 0.64 (0.44–0.81) 0.82 (0.73–0.89) Left 0.46 (0.28–0.66) 0.95 (0.88–0.98) 0.72 (0.47–0.90) 0.86 (0.78–0.92)
NPV, negative predictive value; PPV, positive predictive value; SCXR, supine chest x-ray.
Diagnostic accuracy values for supine chest x-ray readings of basal pneumonia, with results of CT scans serving as a reference standard. Grades for pneumonia on chest x-ray: 0 = no, 1 = possible, 2 = highly suspected. Diagnostic accuracy values are shown both for rating grades 1 and 2 as positive for pneumonia and for rating only grade 2 as positive. For each categorization, diagnostic accuracy values are presented for the reading results without and with comparison to previous examinations, where available. Clopper-Pearson confidence intervals are given in parentheses.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 3
CT Correlates of False-positive Basal Pneumonia Diagnosis on Supine Chest X-Ray
CXR Grading Rated as Positive Comparison to Previous Examination Side False-positive Pneumonia (% of Total) CT Correlate (% of False-positive) None PE AT PE + AT 1 + 2 No Right 27.3 12.8 2.1 19.1 66.0 Left 32.0 7.3 5.5 30.9 56.4 1 + 2 Yes Right 29.8 10.8 2.7 24.3 62.2 Left 32.3 0.0 7.5 32.5 60.0 2 No Right 4.1 14.3 0.0 14.3 71.4 Left 2.3 0.0 0.0 0.0 100.0 2 Yes Right 8.1 10.0 0.0 10.0 80.0 Left 4.0 0.0 0.0 20.0 80.0
AT, atelectasis; CT, computed tomography; PE, pleural effusion; SCXR, supine chest x-ray.
CT correlates of false-positive basal pneumonia diagnosis in supine chest x-ray readings (groups as noted in the caption of Table 2 ).
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 4
Predictors of CT Diagnosis of Pneumonia
Independent variables Right Lung Left Lung OR (95% CI)P Value OR (95% CI)P Value Age 0.99 (0.97–1.02) .654 0.99 (0.96–1.02) .492 Gender 1.46 (0.65–3.28) .356 1.61 (0.70–3.68) .260 CRP level 0.97 (0.93–1.02) .265 0.98 (0.94–1.02) .344 SCXR grading4.71 (2.71–8.16)<.0014.65 (2.52–8.60)<.001
CI, confidence interval; CRP, C-reactive protein; CT, computed tomography; OR, odds ratio; SCXR, supine chest x-ray.
Bold numbers indicate statistical significance. A binary logistic regression analysis was performed for the CT diagnosis of pneumonia.
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Graat M.E., Choi G., Wolthuis E.K., et. al.: The clinical value of daily routine chest radiographs in a mixed medical-surgical intensive care unit is low. Crit Care 2006; 10: pp. R11.
2. Hejblum G., Chalumeau-Lemoine L., Ioos V., et. al.: Comparison of routine and on-demand prescription of chest radiographs in mechanically ventilated adults: a multicentre, cluster-randomised, two-period crossover study. Lancet 2009; 374: pp. 1687-1693.
3. Hendrikse K.A., Gratama J.W., Hove W., et. al.: Low value of routine chest radiographs in a mixed medical-surgical ICU. Chest 2007; 132: pp. 823-828.
4. Krivopal M., Shlobin O.A., Schwartzstein R.M.: Utility of daily routine portable chest radiographs in mechanically ventilated patients in the medical ICU. Chest 2003; 123: pp. 1607-1614.
5. Oba Y., Zaza T.: Abandoning daily routine chest radiography in the intensive care unit: meta-analysis. Radiology 2010; 255: pp. 386-395.
6. Leong C.S., Cascade P.N., Kazerooni E.A., et. al.: Bedside chest radiography as part of a postcardiac surgery critical care pathway: a means of decreasing utilization without adverse clinical impact. Crit Care Med 2000; 28: pp. 383-388.
7. American Thoracic Society, Infectious Diseases Society of America : Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005; 171: pp. 388-416.
8. Tejerina E., Frutos-Vivar F., Restrepo M.I., et. al.: Incidence, risk factors, and outcome of ventilator-associated pneumonia. J Crit Care 2006; 21: pp. 56-65.
9. Leroy O., Meybeck A., d Escrivan T., et. al.: Hospital-acquired pneumonia in critically ill patients: mortality risk stratification upon onset. Treat Respir Med 2004; 3: pp. 123-131.
10. Klompas M.: Does this patient have ventilator-associated pneumonia?. JAMA 2007; 297: pp. 1583-1593.
11. Rea-Neto A., Youssef N.C., Tuche F., et. al.: Diagnosis of ventilator-associated pneumonia: a systematic review of the literature. Crit Care 2008; 12: pp. R56.
12. Hansell D.M., Bankier A.A., MacMahon H., et. al.: Fleischner Society: glossary of terms for thoracic imaging. Radiology 2008; 246: pp. 697-722.
13. Barloon T.J., Galvin J.R., Mori M., et. al.: High-resolution ultrafast chest CT in the clinical management of febrile bone marrow transplant patients with normal or nonspecific chest roentgenograms. Chest 1991; 99: pp. 928-933.
14. Fabregas N., Ewig S., Torres A., et. al.: Clinical diagnosis of ventilator associated pneumonia revisited: comparative validation using immediate post-mortem lung biopsies. Thorax 1999; 54: pp. 867-873.
15. Lefcoe M.S., Fox G.A., Leasa D.J., et. al.: Accuracy of portable chest radiography in the critical care setting. Diagnosis of pneumonia based on quantitative cultures obtained from protected brush catheter. Chest 1994; 105: pp. 885-887.
16. Wunderink R.G., Woldenberg L.S., Zeiss J., et. al.: The radiologic diagnosis of autopsy-proven ventilator-associated pneumonia. Chest 1992; 101: pp. 458-463.
17. Weber C., Maas R., Steiner P., et. al.: Importance of digital thoracic radiography in the diagnosis of pulmonary infiltrates in patients with bone marrow transplantation during aplasia]. Rofo 1999; 171: pp. 294-301.
18. Self W.H., Courtney D.M., McNaughton C.D., et. al.: High discordance of chest x-ray and computed tomography for detection of pulmonary opacities in ED patients: implications for diagnosing pneumonia. Am J Emerg Med 2013; 31: pp. 401-405.
19. Carraro E., Cook C., Evans D., et. al.: Lack of added predictive value of portable chest radiography in diagnosing ventilator-associated pulmonary infection. Surg Infect (Larchmt) 2014; 15: pp. 739-744.
20. Herman P.G., Gerson D.E., Hessel S.J., et. al.: Disagreements in chest roentgen interpretation. Chest 1975; 68: pp. 278-282.
21. Herman P.G., Hessel S.J.: Accuracy and its relationship to experience in the interpretation of chest radiographs. Invest Radiol 1975; 10: pp. 62-67.
22. Albaum M.N., Hill L.C., Murphy M., et. al.: Interobserver reliability of the chest radiograph in community-acquired pneumonia. PORT investigators. Chest 1996; 110: pp. 343-350.
23. Ojutiku O., Haramati L.B., Rakoff S., et. al.: Radiology residents’ on-call interpretation of chest radiographs for pneumonia. Acad Radiol 2005; 12: pp. 658-664.