This brief review of magnetic resonance susceptometry summarizes the methods conceived in the authors’ laboratory during the past several years. This article shows how venous oxygen saturation is quantified in large draining veins by field mapping and how this information, in concert with simultaneous measurement of cerebral blood flow, yields cerebral metabolic rate of oxygen, the brain’s rate of oxygen consumption. The accuracy of this model-based approach in which the blood vessel is approximated as a long, straight cylinder, for which an analytical solution for the induced field exists, is discussed. It is shown that the approach is remarkably robust, allowing for time-resolved quantification of whole-brain metabolism at rest and in response to stimuli, thereby providing detailed information on cerebral physiology in health and disease not previously amenable by noninvasive methods.
The human brain accounts for only 2% of the body’s weight, but 20% of the body’s total energy requirement . This enormous energy demand, necessary to maintain the default mode of brain activity, is incompletely understood. Oxygen consumption, typically quantified as the cerebral metabolic rate of oxygen ( CMRO 2 ), has been measured in various ways, most typically by positron emission tomography, which yielded values on the order of 130 μmol/min per 100 g in the resting awake state. Even during light sleep, CMRO 2 is only insignificantly lower , and only in deep sleep —and more so during anesthesia —is energy demand substantially lower. Further, incremental CMRO 2 increases in response to mental tasks have been found to be minor relative to the brain’s baseline demand. The brain’s default-mode energy demand is satisfied by oxidation of glucose to water and carbon dioxide. The resulting free energy generates adenosine triphosphate (ATP), the body’s universal currency of energy. In contrast, incremental demand during task activation is supplied via the glycolytic pathway of glucose oxidation.
The ratio of the oxygen consumed over the oxygen supplied by blood flow (oxygen extraction fraction [OEF]) has been found to be largely independent of the region of the brain in which it is measured . Even though oxygen consumption of gray matter is four to five times greater than that of white matter, the greater oxygen demand is offset by a commensurate increase in the rate of delivery in the form of cerebral blood flow. Once OEF is known, CMRO 2 can be quantified from a measurement of blood flow by invoking Fick’s principle, typically expressed as:
CMRO2=Ca⋅CBF⋅(SaO2−SvO2) C
M
R
O
2
=
C
a
·
C
B
F
·
(
S
a
O
2
−
S
v
O
2
)
Here, C a is the blood’s oxygen carrying capacity, CBF is the cerebral blood flow, and SaO 2 and SvO 2 are the arterial and venous oxygen saturations, respectively. The difference between arterial and venous oxygen saturation, SaO2−SvO2 S
a
O
2
−
S
v
O
2 , is also referred to as AvO2D A
v
O
2
D , arteriovenous oxygen saturation difference. It is related to oxygen extraction fraction as OEF=AVO2/SaO2 O
E
F
=
A
V
O
2
/
S
a
O
2 and, as long as arterial blood is fully saturated, AvO 2 D = AvO 2 D .
A recent review by Yablonskiy et al. examined the various magnetic resonance imaging (MRI)-based approaches for quantifying OEF, the key parameter that yields CMRO 2 via Equation (1) , along with the underlying theoretical models . In this brief review, we show how whole-brain OEF can be obtained by a quantitative MRI technique that relies on the measurement of the magnetic susceptibility of venous blood in one of the major cerebral veins, which, together with simultaneous measurement of CBF by phase-contrast blood-flow velocimetry, yields CMRO 2 .
Get Radiology Tree app to read full this article<
Principle of MRI susceptometry and alternative approaches to measure SvO 2
Magnetic Properties of Whole Blood
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
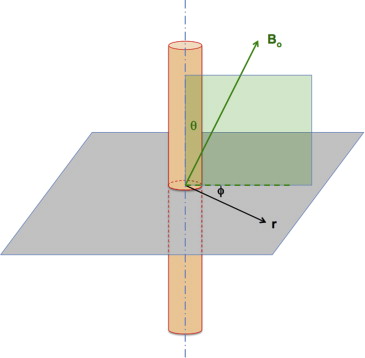
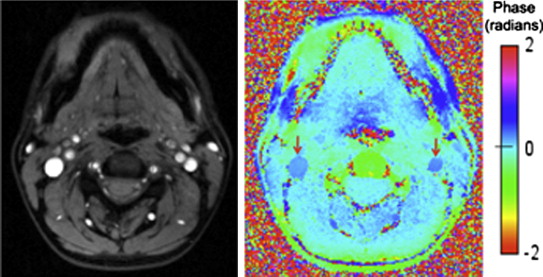
Model-Based Approaches for Quantifying Blood Magnetic Susceptibility: Accuracy and Reproducibility
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
ΔBint=Δχ2(cos2θ−13)B0 Δ
B
int
=
Δ
χ
2
(
co
s
2
θ
−
1
3
)
B
0
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
ΔBext=(Δχ2sin2θ⋅a2r2⋅cos2ϕ)B0 Δ
B
e
x
t
=
(
Δ
χ
2
si
n
2
θ
·
a
2
r
2
·
cos
2
ϕ
)
B
0
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Δχ=Δχdo⋅Hct⋅(1−SvO2) Δ
χ
=
Δ
χ
d
o
·
H
c
t
·
(
1
−
S
v
O
2
)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Δφ(x,y)=γ⋅ΔB⋅ΔTE Δ
φ
(
x
,
y
)
=
γ
·
Δ
B
·
Δ
T
E
in which Δφ(x,y) Δ
φ
(
x
,
y
) is the relative phase at pixel location (x,y) (
x
,
y
) , γ is the gyromagnetic ratio, and ΔTE Δ
T
E is the inter-echo time.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
SvO2=1−2ΔφieγB0⋅ΔTE⋅Δχdo⋅Hct(cos2θ−1/3) S
v
O
2
=
1
−
2
Δ
φ
i
e
γ
B
0
·
Δ
T
E
·
Δ
χ
d
o
·
H
c
t
(
cos
2
θ
−
1
/
3
)
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Numerical Approaches to Obtain Spatially Resolved Susceptibility from Induced Field Maps
Get Radiology Tree app to read full this article<
T 2 -Based Approaches
Get Radiology Tree app to read full this article<
Time-resolved quantification of whole-brain CMRO 2 at rest and in response to stimuli
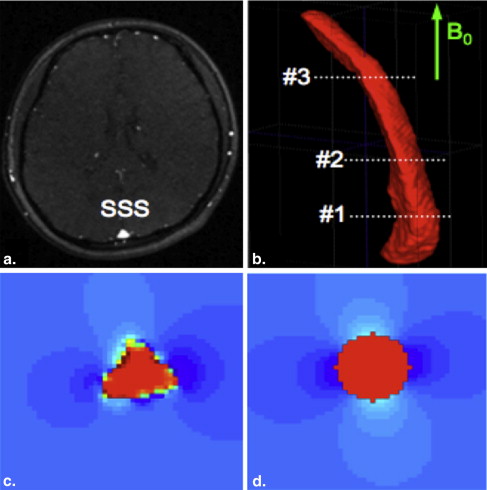
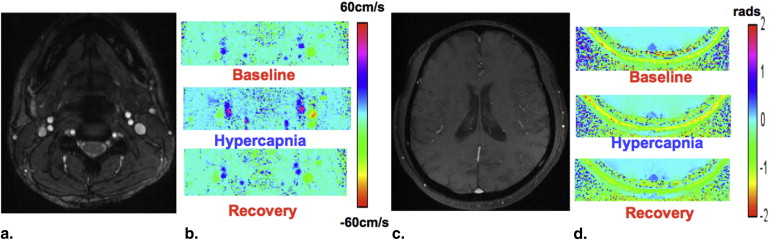
Simultaneous Measurement of Flow and SvO 2
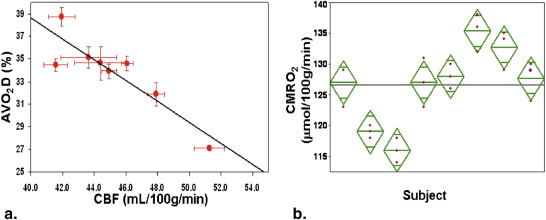
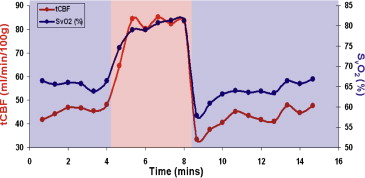
Resting-state CMRO 2 and response to isometabolic stimuli
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Clinical applications to the brain in neonates with congenital heart disease
Get Radiology Tree app to read full this article<
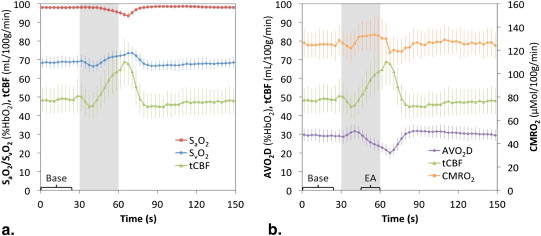
High-Speed CMRO 2 Measurement in Response to Non-Steady-State Stimuli
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusions and future directions
Get Radiology Tree app to read full this article<
References
1. Raichle M.E., Gusnard D.A.: Appraising the brain’s energy budget. Proc Natl Acad Sci U S A 2002; 99: pp. 10237-10239.
2. Raichle M.E., MacLeod A.M., Snyder A.Z., et. al.: A default mode of brain function. Proc Natl Acad Sci U S A 2001; 98: pp. 676-682.
3. Madsen P.L., Schmidt J.F., Holm S., et. al.: Cerebral oxygen metabolism and cerebral blood flow in man during light sleep (stage 2). Brain Res 1991; 557: pp. 217-220.
4. Madsen P.L., Schmidt J.F., Wildschiodtz G., et. al.: Cerebral O2 metabolism and cerebral blood flow in humans during deep and rapid-eye-movement sleep. J Appl Physiol 1991; 70: pp. 2597-2601.
5. Renou A.M., Vernhiet J., Macrez P., et. al.: Cerebral blood flow and metabolism during etomidate anaesthesia in man. Br J Anaesthes 1978; 50: pp. 1047-1051.
6. Yablonskiy DA, Sukstanskii AL, He X. Blood oxygenation level-dependent (BOLD)-based techniques for the quantification of brain hemodynamic and metabolic properties - theoretical models and experimental approaches. NMR Biomed 2013; 26:963–986.
7. Heiss W.D., Huber M., Fink G.R., et. al.: Progressive derangement of periinfarct viable tissue in ischemic stroke. J Cereb Blood Flow Metab 1992; 12: pp. 193-203.
8. Ragan D.K., McKinstry R., Benzinger T., et. al.: Alterations in cerebral oxygen metabolism after traumatic brain injury in children. J Cereb Blood Flow Metab 2013; 33: pp. 48-52.
9. Placidi F., Diomedi M., Cupini L.M., et. al.: Impairment of daytime cerebrovascular reactivity in patients with obstructive sleep apnoea syndrome. J Sleep Res 1998; 7: pp. 288-292.
10. Ishii K., Kitagaki H., Kono M., et. al.: Decreased medial temporal oxygen metabolism in Alzheimer’s disease shown by PET. J Nucl Med 1996; 37: pp. 1159-1165.
11. Girouard H., Iadecola C.: Neurovascular coupling in the normal brain and in hypertension, stroke, and Alzheimer disease. J Appl Physiol 2006; 100: pp. 328-335.
12. Pauling L., Coryell C.D.: The magnetic properties and structure of hemoglobin, oxyhemoglobin and carbonmonoxyhemoglobin. Proc Natl Acad Sci U S A 1936; 22: pp. 210-216.
13. Schenck J.F.: The role of magnetic susceptibility in magnetic resonance imaging: MRI magnetic compatibility of the first and second kinds. Med Phys 1996; 23: pp. 815-850.
14. Haacke E.M., Lai S., Reichenbach J.R., et. al.: In vivo measurement of blood oxygen saturation using magnetic resonance imaging: a direct validation of the blood oxygen level-dependent concept in functional brain imaging. Human Brain Mapp 1997; 5: pp. 341-346.
15. Fernández-Seara M.A., Techawiboonwong A., Detre J.A., et. al.: MR susceptometry for measuring global brain oxygen extraction. Magn Res Med 2006; 55: pp. 967-973.
16. Thulborn K.R., Waterton J.C., Matthews P.M., et. al.: Oxygenation dependence of the transverse relaxation time of the water protons in whole blood at high field. Biochim Biophys Acta 1982; 714: pp. 265-270.
17. Wright G.A., Hu B.S., Macovski A.: Estimating oxygen saturation of blood in vivo with MR imaging at 1.5 T. 1991 I.I. Rabi Award J Magn Reson Imaging 1991; 1: pp. 275-283.
18. Nield L.E., Qi X., Yoo S.J., et. al.: MRI-based blood oxygen saturation measurements in infants and children with congenital heart disease. Pediatr Radiol 2002; 32: pp. 518-522.
19. Xu F., Ge Y., Lu H.: Noninvasive quantification of whole-brain cerebral metabolic rate of oxygen (CMRO2) by MRI. Magn Res Med 2009; 62: pp. 141-148.
20. Reichenbach J.R., Haacke E.M.: High-resolution BOLD venographic imaging: a window into brain function. NMR Biomed 2001; 14: pp. 453-467.
21. Weisskoff R.M., Kiihne S.: MRI susceptometry: image-based measurement of absolute susceptibility of MR contrast agents and human blood. Magn Reson Med 1992; 24: pp. 375-383.
22. Spees W.M., Yablonskiy D.A., Oswood M.C., et. al.: Water proton MR properties of human blood at 1.5 Tesla: magnetic susceptibility, T(1), T(2), T*(2), and non-Lorentzian signal behavior. Magn Reson Med 2001; 45: pp. 533-542.
23. Jain V., Abdulmalik O., Propert K.J., et. al.: Investigating the magnetic susceptibility properties of fresh human blood for noninvasive oxygen saturation quantification. Magn Reson Med 2012; 68: pp. 863-867.
24. Langham M.C., Magland J.F., Epstein C.L., et. al.: Accuracy and precision of MR blood oximetry based on the long paramagnetic cylinder approximation of large vessels. Magn Reson Med 2009; 62: pp. 333-340.
25. Langham M.C., Magland J.F., Floyd T.F., et. al.: Retrospective correction for induced magnetic field inhomogeneity in measurements of large-vessel hemoglobin oxygen saturation by MR susceptometry. Magn Reson Med 2009; 61: pp. 626-633.
26. Li C., Langham M.C., Epstein C.L., et. al.: Accuracy of the cylinder approximation for susceptometric measurement of intravascular oxygen saturation. Magn Reson Med 2012; 67: pp. 808-813.
27. Jenkinson M., Wilson J.L., Jezzard P.: Perturbation method for magnetic field calculations of nonconductive objects. Magn Reson Med 2004; 52: pp. 471-477.
28. Jain V., Langham M.C., Wehrli F.W.: MRI estimation of global brain oxygen consumption rate. J Cerebr Blood Flow Metab 2010; 30: pp. 1598-1607.
29. de Rochefort L., Brown R., Prince M.R., et. al.: Quantitative MR susceptibility mapping using piece-wise constant regularized inversion of the magnetic field. Magn Reson Med 2008; 60: pp. 1003-1009.
30. Schweser F., Deistung A., Lehr B.W., et. al.: Quantitative imaging of intrinsic magnetic tissue properties using MRI signal phase: an approach to in vivo brain iron metabolism?. Neuroimage 2011; 54: pp. 2789-2807.
31. Fan A., Bilgic B., Gagnon L., et. al.: Quantitative oxygenation venography from MRI phase. Proc Intl Soc Mag Reson Med 2013; 21: pp. 3721.
32. Xu F., Liu P., Pascual J.M., et. al.: Effect of hypoxia and hyperoxia on cerebral blood flow, blood oxygenation, and oxidative metabolism. J Cerebr Blood Flow Metab 2012; 32: pp. 1909-1918.
33. Xu F., Uh J., Brier M.R., et. al.: The influence of carbon dioxide on brain activity and metabolism in conscious humans. J Cerebr Blood Flow Metab 2011; 31: pp. 58-67.
34. Xu F., Uh J., Liu P., et. al.: On improving the speed and reliability of T(2) -relaxation-under-spin-tagging (TRUST) MRI. Magn Reson Med 2012; 68: pp. 198-204.
35. Jain V., Magland J., Langham M., et. al.: High temporal resolution in vivo blood oximetry via projection-based T(2) measurement. Magn Reson Med 2012 October 18;
36. Ibaraki M., Miura S., Shimosegawa E., et. al.: Quantification of cerebral blood flow and oxygen metabolism with 3-dimensional PET and 15O: validation by comparison with 2-dimensional PET. J Nucl Med 2008; 49: pp. 50-59.
37. Jain V., Jain G., Magland J., et. al.: Regional cerebral metabolic rate of oxygen consumption in the middle cerebral artery territory. Proc Intl Soc Mag Reson Med 2011; pp. 2436. Montreal, Canada: ISMRM
38. Fan A.P., Benner T., Bolar D.S., et. al.: Phase-based regional oxygen metabolism (PROM) using MRI. Magn Reson Med 2012; 67: pp. 669-678.
39. Jain V., Langham M.C., Floyd T.F., et. al.: Rapid magnetic resonance measurement of global cerebral metabolic rate of oxygen consumption in humans during rest and hypercapnia. J Cerebr Blood Flow Metab 2011; 31: pp. 1504-1512.
40. Chen J.J., Pike G.B.: Global cerebral oxidative metabolism during hypercapnia and hypocapnia in humans: implications for BOLD fMRI. J Cerebr Blood Flow Metab 2010; 30: pp. 1094-1099.
41. Leenders K.L., Frackowiak R.S., Quinn N., et. al.: Brain energy metabolism and dopaminergic function in Huntington’s disease measured in vivo using positron emission tomography. Movement Disord 1986; 1: pp. 69-77.
42. Tanaka M., Kondo S., Okamoto K., et. al.: Cerebral perfusion and oxygen metabolism in Parkinson’s disease: positron emission tomographic study using oxygen-15-labeled CO2 and O2. Nihon Rinsho 1997; 55: pp. 218-221.
43. Rodgers Z.B., Jain V., Englund E.K., et. al.: High temporal resolution MRI quantification of global cerebral metabolic rate of oxygen consumption in response to apneic challenge. J Cereb Blood Flow Metab 2013; 33: pp. 1514-1522.
44. Thomason M.E., Foland L.C., Glover G.H.: Calibration of BOLD fMRI using breath holding reduces group variance during a cognitive task. Human Brain Mapp 2007; 28: pp. 59-68.
45. Duchna H.W., Guilleminault C., Stoohs R.A., et. al.: Vascular reactivity in obstructive sleep apnea syndrome. Am J Resp Crit Care Med 2000; 161: pp. 187-191.
46. Virtanen J., Noponen T., Salmi T., et. al.: Impaired cerebral vasoreactivity may cause cerebral blood volume dip following obstructive sleep apnea termination. Sleep Breath 2011; 16: pp. 309-312.
47. Van Zijl P.C., Hua J., Lu H.: The BOLD post-stimulus undershoot, one of the most debated issues in fMRI. NeuroImage 2012; 62: pp. 1092-1102.
48. Hua J., Stevens R.D., Huang A.J., et. al.: Physiological origin for the BOLD poststimulus undershoot in human brain: vascular compliance versus oxygen metabolism. J Cerebr Blood Flow Metab 2011; 31: pp. 1599-1611.