Rationale and Objectives
Falls are a common cause of emergency department (ED) visits in the United States. We evaluated trends in computed tomography (CT) utilization for pediatric fall victims in the United States from 2001 to 2010.
Materials and Methods
Using the National Hospital Ambulatory Medical Care Survey from 2001 to 2010, we identified all visits of pediatric (aged <18 years) patients presenting to EDs after falls. This database surveys approximately 500 EDs per year for 4 weeks providing national estimates on ED resource utilization and outcomes. We studied trends in CT utilization and proportion of visits with life-threatening conditions after falls. We also studied the association between CT utilization rates and demographic characteristics and admission status.
Results
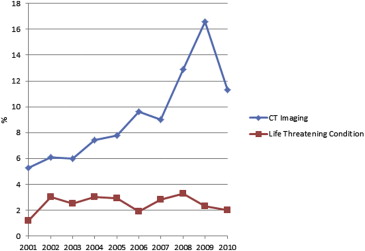
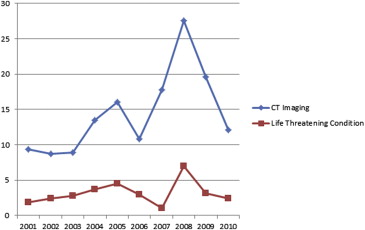
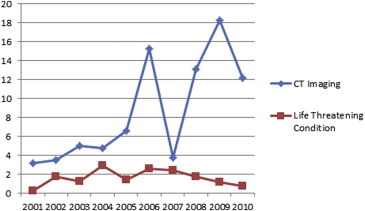
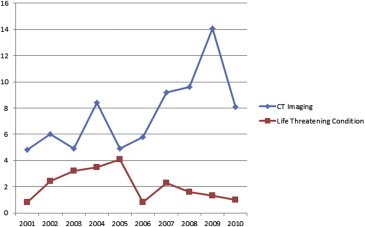
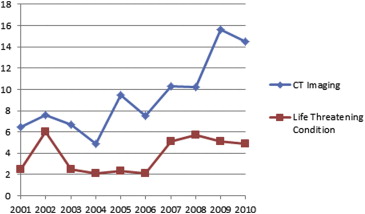
A total of 9763 unweighted observations for a total of 32,432,686 pediatric fall patients were seen in US EDs from 2001 to 2010. The proportion of pediatric fall patients receiving CT increased from 5.3% in 2001 to a peak of 16.6% in 2009 and decreased to 11.3% in 2010, whereas the proportion of pediatric fall patients with life-threatening conditions fluctuated between 1.2% and 3.3% during this period. In multivariate logistic regression analysis, each increasing year was independently associated with CT utilization (odds ratio [OR], 1.15; 95% confidence interval [CI], 1.14–1.16). Patients aged 0–1 years had higher odds of CT utilization than patients aged 13–17 years (OR, 2.27; 95% CI, 2.26–2.27).
Conclusions
There was a twofold increase in CT utilization among pediatric fall visits from 2001 to 2010. When controlling for demographic and clinical variables, increasing year was independently associated with CT utilization. These findings suggest that CT may be overutilized among pediatric fall patients.
Computed tomography (CT) utilization in the pediatric population has seen a rapid increase over the past decade in pediatric emergency departments (EDs) . It is estimated that at least 4 million CT scans are conducted each year on children in the United States . Diagnostic capability, wider availability, and prompt results make CT a preferred method of imaging in EDs across the United States . Falls account for the most ED visits in the pediatric population with relatively high rates of morbidity and mortality .
Recent studies indicate that nearly a quarter of all CTs ordered are inappropriate, thus subjecting patients to unnecessary radiation exposure . This is particularly concerning in the pediatric population, placing them at a potential risk for cancer, a risk that is cumulative over the patient’s lifetime . Furthermore, unnecessary imaging is a significant contributor to the rising cost of health care in the United States . Because of these issues of safety and inappropriate use and cost, we undertook a study to evaluate CT utilization trends in the pediatric population and study the associated demographic and clinical features.
Material and methods
Patient Population
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Outcomes
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Results
Patient Population
Get Radiology Tree app to read full this article<
Table 1
Univariate Analysis of Variables Associated with Computed Tomography Imaging
Attribute Patients Presenting with Fall, N (%) Presenting with Fall Who Are Also Receiving CT Imaging, N (%) Odds Ratio (95% Confidence Interval) Age (years) 0–1 4,716,880 (14.4) 684,887 (14.5) 1.56 (1.55–1.56) 2–5 9,238,272 (28.3) 804,689 (8.7) 0.93 (0.92–0.93) 6–12 11,379,168 (34.8) 873,404 (7.7) 0.81 (0.81–0.81) 13–17 7,324,462 (22.4) 683,347 (9.3) Ref Gender Female 13,192,248 (40.4) 1,260,621 (9.6) Male 19,466,534 (59.6) 1,785,706 (9.2) 0.96 (0.95–0.96) Insurance status Private 16,719,694 (52.8) 1,618,127 (9.7) Ref Medicaid 10,281,238 (32.5) 953,315 (9.3) 0.95 (0.95–0.96) Self-pay 2,711,403 (8.6) 204,450 (7.5) 0.76 (0.76–0.76) Ethnicity White 22,407,019 (68.6) 2,094,860 (9.4) Ref Black 5,631,363 (17.2) 479,026 (8.5) 0.90 (0.90–0.90) Hispanic 3,397,591 (10.4) 348,655 (10.3) 1.11 (1.10–1.11) Other 1,222,809 (3.7) 123,786 (10.1) 1.09 (1.08–1.10) Admission No 32,109,068 (98.3) 2,884,419 (9.0) 4.23 (4.21–4.26) Yes 549,714 (1.7) 161,908 (29.5) Life-threatening injury No 31843166 (97.5) 2763996 (8.7) 5.57 (5.54–5.60) Yes 815616 (2.5) 282331 (34.6) Arrival method No ambulance 17983261 (93.2) 1437118 (8.0) 2.90 (2.89–2.91) Ambulance 1310740 (6.8) 263712 (20.1)
Get Radiology Tree app to read full this article<
Trends in CT Utilization and Hospital Admission
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Variables Associated with CT Utilization
Get Radiology Tree app to read full this article<
Table 2
Multivariate Analysis
Attribute Odds Ratio (95% Confidence Interval) ∗ Age (years) 0–1 2.27 (2.26–2.27) 2–5 1.01 (1.01–1.02) 6–12 0.92 (0.92–0.93) 13–17 Ref Male versus female 0.86 (0.86–0.86) Insurance status Private Ref Medicaid 0.90 (0.89–0.90) Self-pay 0.55 (0.55–0.55) Ethnicity White Ref Black 0.98 (0.98–0.99) Hispanic 1.14 (1.14–1.15) Other 1.14 (1.13–1.15) Arrival in ambulance 2.30 (2.29–2.31) Admitted versus not admitted 3.25 (3.22–3.28) Year (unit change) 1.15 (1.14–1.16) Year (over range) 2.21 (2.20–2.22) Life-threatening condition 3.78 (3.76–3.80)
Analysis adjusted for age, gender, insurance status, ethnicity, arrival in ambulance, hospital admission, year, and presence of life-threatening condition.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Limitations
Get Radiology Tree app to read full this article<
Conclusions
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Broder J., Fordham L.A., Warshauer D.M.: Increasing utilization of computed tomography in the pediatric emergency department, 2000-2006. Emerg Radiol 2007; 14: pp. 227-232.
2. Brenner D.J., Hall E.J.: Computed tomography—an increasing source of radiation exposure. The New England journal of medicine 2007; 357: pp. 2277-2284.
3. Broder J.S.: CT utilization: the emergency department perspective. Pediatr Radiol 2008; 38: pp. S664-S669.
4. Lee J., Kirschner J., Pawa S., et. al.: Computed tomography use in the adult emergency department of an academic urban hospital from 2001 to 2007. Ann Emerg Med 2010; 56: pp. 591-596.
5. Boone J.M., Brunberg J.A.: Computed tomography use in a tertiary care university hospital. J Am Coll Radiol 2008; 5: pp. 132-138.
6. Sosna J., Slasky B.S., Bar-Ziv J.: Computed tomography in the emergency department. Am J Emerg Med 1997; 15: pp. 244-247.
7. Wang M.Y., Kim K.A., Griffith P.M., et. al.: Injuries from falls in the pediatric population: an analysis of 729 cases. J Pediatr Surg 2001; 36: pp. 1528-1534.
8. Hall J.R., Reyes H.M., Horvat M., et. al.: The mortality of childhood falls. J Trauma 1989; 29: pp. 1273-1275.
9. Kraus J.F., Fife D., Cox P., et. al.: Incidence, severity, and external causes of pediatric brain injury. Am J Dis Child 1986; 140: pp. 687-693.
10. Mathers L.J., Weiss H.B.: Incidence and characteristics of fall-related emergency department visits. Acad Emerg Med 1998; 5: pp. 1064-1070.
11. Lehnert B.E., Bree R.L.: Analysis of appropriateness of outpatient CT and MRI referred from primary care clinics at an academic medical center: how critical is the need for improved decision support?. J Am Coll Radiol 2010; 7: pp. 192-197.
12. Flynn T.W., Smith B., Chou R.: Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good. J Orthop Sports Phys Ther 2011; 41: pp. 838-846.
13. Berrington de Gonzalez A., Mahesh M., Kim K.P., et. al.: Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med 2009; 169: pp. 2071-2077.
14. Fazel R., Krumholz H.M., Wang Y., et. al.: Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009; 361: pp. 849-857.
15. Frush D.P., Donnelly L.F., Rosen N.S.: Computed tomography and radiation risks: what pediatric health care providers should know. Pediatrics 2003; 112: pp. 951-957.
16. Karlsson P., Holmberg E., Lundell M., et. al.: Intracranial tumors after exposure to ionizing radiation during infancy: a pooled analysis of two Swedish cohorts of 28,008 infants with skin hemangioma. Radiat Res 1998; 150: pp. 357-364.
17. Pearce M.S., Salotti J.A., Little M.P., et. al.: Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380: pp. 499-505.
18. Smith-Bindman R., Miglioretti D.L., Larson E.B.: Rising use of diagnostic medical imaging in a large integrated health system. Health Aff (Millwood) 2008; 27: pp. 1491-1502.
19. Eaton D.K., Kann L., Kinchen S., et. al.: Youth risk behavior surveillance—United States, 2011. MMWR Surveill Summ 2012; 61: pp. 1-162.
20. Larson D.B., Johnson L.W., Schnell B.M., et. al.: Rising use of CT in child visits to the emergency department in the United States, 1995-2008. Radiology 2011; 259: pp. 793-801.
21. Roudsari B., Moore D.S., Jarvik J.G.: Trend in the utilization of CT for adolescents admitted to an adult level I trauma center. J Am Coll Radiol 2010; 7: pp. 796-801.
22. Blackwell C.D., Gorelick M., Holmes J.F., et. al.: Pediatric head trauma: changes in use of computed tomography in emergency departments in the United States over time. Annals of Emergency Medicine 2007; 49: pp. 320-324.
23. Adelgais K.M., Browne L., Holsti M., et. al.: Cervical spine computed tomography utilization in pediatric trauma patients. J Pediatr Surg 2014; 49: pp. 333-337.
24. Tsze D.S., Asnis L.M., Merchant R.C., et. al.: Increasing computed tomography use for patients with appendicitis and discrepancies in pain management between adults and children: an analysis of the NHAMCS. Annals of Emergency Medicine 2012; 59: pp. 395-403.
25. Hoshiko S., Smith D., Fan C., et. al.: Trends in CT scan rates in children and pregnant women: teaching, private, public and nonprofit facilities. Pediatr Radiol 2014; 44: pp. 522-528.
26. Oh H.Y., Kim E.Y., Kim J.E., et. al.: Trends of CT use in the pediatric emergency department in a tertiary academic hospital of Korea during 2001–2010. Korean J Radiol 2012; 13: pp. 771-775.
27. Lee C.I., Haims A.H., Monico E.P., et. al.: Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology 2004; 231: pp. 393-398.
28. Babl F.E., Lyttle M.D., Bressan S., et. al.: A prospective observational study to assess the diagnostic accuracy of clinical decision rules for children presenting to emergency departments after head injuries (protocol): the Australasian Paediatric Head Injury Rules Study (APHIRST). BMC Pediatr 2014; 14: pp. 148.
29. Hess E.P., Wyatt K.D., Kharbanda A.B., et. al.: Effectiveness of the head CT choice decision aid in parents of children with minor head trauma: study protocol for a multicenter randomized trial. Trials 2014; 15: pp. 253.
30. Bressan S., Romanato S., Mion T., et. al.: Implementation of adapted PECARN decision rule for children with minor head injury in the pediatric emergency department. Acad Emerg Med 2012; 19: pp. 801-807.
31. Hershkovitz Y., Zoarets I., Stepansky A., et. al.: Computed tomography is not justified in every pediatric blunt trauma patient with a suspicious mechanism of injury. Am J Emerg Med 2014; 32: pp. 697-699.
32. Schachar J.L., Zampolin R.L., Miller T.S., et. al.: External validation of the New Orleans Criteria (NOC), the Canadian CT Head Rule (CCHR) and the National Emergency X-Radiography Utilization Study II (NEXUS II) for CT scanning in pediatric patients with minor head injury in a non-trauma center. Pediatr Radiol 2011; 41: pp. 971-979.
33. Cooper R.J.: NHAMCS: does it hold up to scrutiny?. Annals of Emergency Medicine 2012; 60: pp. 722-725.
34. McCaig L.F., Burt C.W., Schappert S.M., et. al.: NHAMCS: does it hold up to scrutiny?. Annals of Emergency Medicine 2013; 62: pp. 549-551.