Rationale and Objectives
This study is conducted to estimate the sensitivity of stereotactic directional vacuum-assisted breast biopsy (ST DVAB) using Bayesian modeling and to predict how many more cancers can be inferred from those lesions without surgical correlation.
Materials and methods
We retrospectively reviewed the 103 lesions from 84 women who underwent ST DVAB. The study was approved by the Institutional Review Board of our hospital. We estimated the sensitivity and prevalence of the study population for ST DVAB by two types of approaches: for the type I approach, the gold standards were surgical correlation or postbiopsy mammographic follow-up. For the type II approach using Bayesian modeling by a beta-binomial model, the only gold standard was surgical correlation and the predicted number of cancerous lesions in those patients without surgical correlation was estimated.
Results
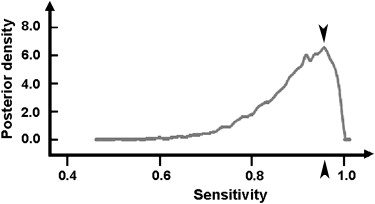
For the type I approach, the sensitivity was 92.3%, and the prevalence 12.6%. For the type II approach, the mean sensitivity of ST DVAB was 89%, and the mean prevalence was 15%. We predicted that an average of 1.7 cancerous lesions occurred among those lesions without surgical correlation by the Bayesian estimation.
Conclusions
The mean sensitivity of ST DVAB using the Bayesian (type II) approach was lower than that using the type I approach, because we regarded the surgery as the only gold standard in Bayesian modeling and the nonoperated lesions were thought to be with unknown true disease status. The Bayesian approach is thus more appropriate to use than the type I approach when the gold standard is incomplete.
Stereotactic directional vacuum-assisted breast biopsy (ST DVAB) is the standard biopsy method for mammographically visible lesions of a suspicious nature, because it has high sensitivity diagnosing breast carcinoma, according to many reported studies . When ST DVAB yields benign pathology concordant with mammographic findings, mammographic follow-up is the recommended management . The lesions are presumed benign if the postbiopsy findings are unchanged for at least 2 years on mammography . However, for lesions showing benign result on ST biopsy, an inherent missed diagnosis is possible with the false-negative (FN) rate ranging from 1.2% to 4.3% . However, for most clinical settings, the sensitivity of ST DVAB was estimated from patients who undergo subsequent surgery or regular mammographic follow-up and is defined as the cancers disclosed by ST DVAB divided by cancers by ST DVAB and subsequent surgery, which did not consider the possible FN lesions in those who received only mammographic follow-up but without surgical correlation. The true disease status of these presumably benign lesions may not be known. Therefore, ST DVAB can be thought as an accurate biopsy method, but may not be regarded as the gold standard for tissue proof, when compared with surgery.
In the literature, Bayesian modeling has been used to estimate the diagnostic test sensitivity and specificity when the gold standard is incomplete and available for only part of the population or not available at all . We used a Bayesian approach to estimate the sensitivity of ST DVAB on the basis of the information for all lesions with or without known true disease status (that is, surgical correlation), and to estimate how many of the nonoperated ST DVAB findings could be inherent cancers when the stricter standard was applied using Bayesian modeling.
Materials and methods
Patients
Get Radiology Tree app to read full this article<
Procedures
Get Radiology Tree app to read full this article<
Postbiopsy clinical course
Get Radiology Tree app to read full this article<
Data collection and analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 1
Correlation of ST DVAB Results and the True Disease Status, Presented in a 2 × 2 Table using Bayesian Estimation
Disease + Disease − Total DVAB+ MPDP + Y1 A− (MPDP + Y1) A DVAB– MNDP + Y2 B− (MNDP + Y2) ∗ B Total (MPDP)+(MNDP + Y2) (A + B)-(MPDP + MNDP + Y2) A + B
Y1: the latent data (without surgical correlation) of true-positive lesions (Y1 = 0); DVAB+: lesions with malignant result on ST DVAB; DVAB−: lesions with non-malignant result (benign or high-risk lesions) on ST DVAB; disease+: malignant lesions; disease−: lesions that are not malignant; MPDP: observed data (with surgical correlation) of mammotome-positive (DVAB+) and disease-positive lesions (true positive); MNDP: observed data of mammotome-negative (DVAB−), but disease-positive lesions (false-negative); Y2: the latent data of cancerous lesions in those lesions without surgical correlation;
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Get Radiology Tree app to read full this article<
Table 2
Correlation of BI-RADS Categories for Lesions and the Corresponding ST DVAB Pathologic Results
BI-RADS Lesion ST DVAB Pathology High-risk Lesions † Categories Benign DCIS ‡ 2 1 0 0 4A 64 2 1 4B 21 2 6 4C 1 0 5
ST DVAB, stereotactic directional vacuum-assisted breast biopsy; BI-RADS, Breast Imaging Reporting and Data System; DCIS, ductal carcinoma in situ.
Fisher’s exact test, P < .0001.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 3
Brief Summary of the Different Types of Lesions in the Bayesian Estimation
Type Number (%) MNDN ∗ 7 (6.8) MNDP 1 (1.0) MNDU ∗∗ 83 (80.6) MPDP 12 (11.6) Total 103 (100)
The expanded terms for MNDN, MNDP, MNDU, and MPDP are the same as in Table 1 .
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Table 4
Diagnostic Performance of ST DVAB for 103 Lesions using Bayesian Estimation
Mean SD 95% CI † Sensitivity 0.891 0.078 (0.697, 0.990) Y2 1.71 2.02 (0.0, 7.0) Pre ∗ 0.150 0.040 (0.082, 0.237)
SD: standard deviation
Y2: the number of cancerous lesions in those non-operated lesions (same meaning as that in Table 1 ).
The convergence of Markov chain Monte Carlo Gibbs sampling was monitored by the Gelman-Rubin convergence statistic and the results indicated that the samples of all the parameters listed in the table had convergence of R to 1.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Appendix
Bayesian program codes
Model
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Pfarl G., Helbich T.H., Riedl C.C., et. al.: Stereotactic 11-gauge vacuum-assisted breast biopsy: A validation study. AJR Am J Roentgenol 2002; 179: pp. 1503-1507.
2. Lomoschitz F.M., Helbich T.H., Rudas M., et. al.: Stereotactic 11-gauge vacuum-assisted breast biopsy: influence of number of specimens on diagnostic accuracy. Radiology 2004; 232: pp. 897-903.
3. Liberman L.: Clinical management issues in percutaneous core breast biopsy. Radiol Clin North Am 2000; 38: pp. 791-807.
4. Liberman L., Kaplan J.B., Morris E.A., et. al.: To excise or to sample the mammographic target: what is the goal of stereotactic 11-gauge vacuum-assisted breast biopsy?. AJR Am J Roentgenol 2002; 179: pp. 679-683.
5. Lee C.H., Philpotts L.E., Horvath L.J., et. al.: Follow-up of breast lesions diagnosed as benign with stereotactic core-needle biopsy: frequency of mammographic change and false-negative rate. Radiology 1999; 212: pp. 189-194.
6. Jackman R.J., Nowels K.W., Rodriguez-Soto J., et. al.: Stereotactic, automated, large-core needle biopsy of nonpalpable breast lesions: false-negative and histologic underestimation rates after long-term follow-up. Radiology 1999; 210: pp. 799-805.
7. Burns R.P., Brown J.P., Roe S.M., et. al.: Stereotactic core-needle breast biopsy by surgeons. Minimum 2-year follow-up of benign lesions. Ann Surg 2000; 232: pp. 542-547.
8. Joseph L., Gyorkos T.W., Coupal L.: Bayesian estimation of disease prevalence and the parameters of diagnostic tests in the absence of a gold standard. Am J Epidemiol 1995; 141: pp. 263-272.
9. Branscum A.J., Gardner I.A., Johnson W.O.: Estimation of diagnostic-test sensitivity and specificity through Bayesian modeling. Prevent Veterinary Med 2005; 68: pp. 145-163.
10. Enøe C., Georgiadis M.P., Johnson W.O.: Estimation of sensitivity and specificity of diagnostic tests and disease prevalence when the true disease state is unknown. Prevent Veterinary Med 2000; 45: pp. 61-81.
11. American College of Radiology: Breast imaging reporting and data system (BI-RADS).4th ed2003.American College of RadiologyReston, Va
12. Rosner B.: Estimation.Rosner B.Fundamentals of biostatistics.2006.Thomson Brooks/ColeBelmont, Ca:pp. 166-225.
13. Rosner B.: Probability.Rosner B.Fundamentals of biostatistics.2006.Thomson Brooks/ColeBelmont, Ca:pp. 43-80.
14. Irfan K., Brem R.F.: Surgical and mammographic follow-up of papillary lesions and atypical lobular hyperplasia diagnosed with stereotactic vacuum-assisted biopsy. Breast J 2002; 8: pp. 230-233.
15. Foster M.C., Helvie M.A., Gregory N.E., et. al.: Lobular carcinoma in situ or atypical lobular hyperplasia at core-needle biopsy: is excisional biopsy necessary?. Radiology 2004; 231: pp. 813-819.
16. Jackman R.J., Birdwell R.L., Ikeda D.M.: Atypical ductal hyperplasia: can some lesions be defined as probably benign after stereotactic 11-gauge vacuum-assisted biopsy, eliminating the recommendation for surgical excision?. Radiology 2002; 224: pp. 548-554.
17. Philpotts L.E., Shaheen N.A., Jain K.S., et. al.: Uncommon high-risk lesions of the breast diagnosed at stereotactic core-needle biopsy: clinical importance. Radiology 2000; 216: pp. 831-837.
18. Mercado C.L., Hamele-Bena D., Oken S.M., et. al.: Papillary lesions of the breast at percutaneous core-needle biopsy. Radiology 2006; 238: pp. 801-808.
19. Sydnor M.K., Wilson J.D., Hijaz T.A., et. al.: Underestimation of the presence of breast carcinoma in papillary lesions initially diagnosed at core-needle biopsy. Radiology 2007; 242: pp. 58-62.
20. Georgian-Smith D., D’Orsi C., Morris E., et. al.: Stereotactic biopsy of the breast using an upright unit, a vacuum-suction needle, and a lateral arm-support system. AJR Am J Roentgenol 2002; 178: pp. 1017-1024.
21. Reynolds H.E., Poon C.M., Goulet R.J., et. al.: Biopsy of breast microcalcifications using an 11-gauge directional vacuum-assisted device. AJR Am J Roentgenol 1998; 171: pp. 611-613.
22. Shen Y.C., Chang C.J., Hsu C., et. al.: Significant difference in the trends of female breast cancer incidence between Taiwanese and Caucasian Americans: implications from age-period-cohort analysis. Cancer Epidemiol Biomarkers Prev 2005; 14: pp. 1986-1990.
23. Leung G.M., Thach T., Lam T.H., et. al.: Trends in breast cancer incidence in Hong Kong between 1973 and 1999: an age-period-cohort analysis. Br J Cancer 2002; 87: pp. 982-988.