Rationale and Objectives
This study aimed to review the current understanding and capabilities regarding use of imaging for noninvasive lesion characterization and its relationship to lung cancer screening and treatment.
Materials and Methods
Our review of the state of the art was broken down into questions about the different lung cancer image phenotypes being characterized, the role of imaging and requirements for increasing its value with respect to increasing diagnostic confidence and quantitative assessment, and a review of the current capabilities with respect to those needs.
Results
The preponderance of the literature has so far been focused on the measurement of lesion size, with increasing contributions being made to determine the formal performance of scanners, measurement tools, and human operators in terms of bias and variability. Concurrently, an increasing number of investigators are reporting utility and predictive value of measures other than size, and sensitivity and specificity is being reported. Relatively little has been documented on quantitative measurement of non-size features with corresponding estimation of measurement performance and reproducibility.
Conclusions
The weight of the evidence suggests characterization of pulmonary lesions built on quantitative measures adds value to the screening for, and treatment of, lung cancer. Advanced image analysis techniques may identify patterns or biomarkers not readily assessed by eye and may also facilitate management of multidimensional imaging data in such a way as to efficiently integrate it into the clinical workflow.
Introduction
Classic methods of image interpretation for early detection of lung cancer are based on lesion measurement and growth . More recently, investigators have published much on the utility and methods of lesion volumetry in multiple settings . In parallel, various measures other than size have long been proposed . This review explores the perspective that advanced image analysis techniques can identify and quantify imaging biomarkers, including but not limited to size, will likely offer great assistance to clinicians in assessing lesions. Taking the view that a systematic rather than ad hoc approach to quantitative analysis of imaging features grounded in an understanding of tumor biology will yield the most useful tools and approaches, we organize our review by first considering the biology to define the assessment or measurement task, identify the requirements for the settings in which this task is undertaken, and summarize the current state of the art with respect to these settings.
Lung cancer begins with neoplastic tissue arising within the cells of the airway of the lung. Primary lung cancer can be divided into two main groups: small cell lung cancers (SCLC) and non–small cell lung cancers. This grouping is done for therapeutic purposes, and the difference is also reflected by the standard “Tumor-Node-Metastasis” staging paradigm . The names are derived from histopathologic presentation:
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
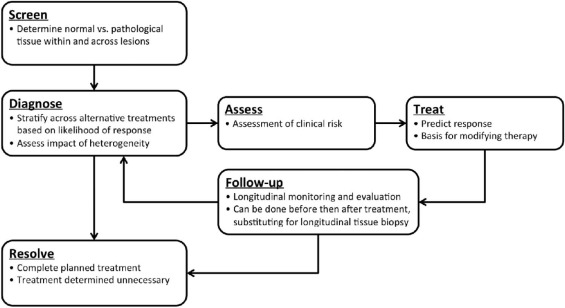
The Role of Imaging for Lung Cancer
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Imaging’s Role in Cancer Screening
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 1
Summary of Fleischner Society Guidelines \*
Nodule type (assessed with contiguous CT sections of ≤1 mm) RecommendationSolitary pure GGO ≤5 mm No follow up >5 mm Follow up with CT at 3 months, and then yearly monitoring for a minimum of 3 years if persistent and unchanged. (FDG-PET is of limited value and therefore not recommended)Subsolid GGOs <5 mm Follow up with CT at 3 months to confirm persistence. If persistent and solid measuring <5 mm, then yearly CT monitoring for a minimum of 3 years ≥5 mm Follow up with CT at 3 months to confirm persistence. If persistent and solid measuring ≥5 mm, then biopsy or surgical resection should be considered. If subsolid nodules measure >10 mm FDG PET should be considered for further evaluationMultiple subsolid nodules Pure GGOs ≤5 mm Follow up with CT at 3 months to confirm persistence. Follow up CT at 2 and 4 years to monitor. If persistent and solid measuring <5 mm, then yearly CT monitoring for a minimum of 3 years Pure GGOs >5 mm with no dominant lesion Follow up with CT at 3 months to confirm persistence. If persistent biopsy or surgical resection should be considered, especially if lesion has a >5 mm solid component
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Imaging’s Role in Cancer Treatment
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Requirements for Increasing the Value of Imaging
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
What Is Currently Attainable with Imaging
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
References
1. Buckler A.J., Mulshine J.L., Gottlieb R., et. al.: The use of volumetric CT as an imaging biomarker in lung cancer. Acad Radiol 2010; 17: pp. 100-106.
2. Buckler A.J., Mozley P.D., Schwartz L., et. al.: Volumetric CT in lung cancer: an example for the qualification of imaging as a biomarker. Acad Radiol 2010; 17: pp. 107-115.
3. Mozley P.D., Schwartz L.H., Bendtsen C., et. al.: Change in lung tumor volume as a biomarker of treatment response: a critical review of the evidence. Ann Oncol 2010; 21: pp. 1751-1755.
4. Buckler A.J.: A procedural template for the qualification of imaging as a biomarker, using volumetric CT as an example.IEEE applied imagery pattern recognition workshop.2009.Cosmos ClubWashington, DC:pp. 7.
5. Buckler A.J., Schwartz L.H., Petrick N., et. al.: Data sets for the qualification of CT as a quantitative imaging biomarker in lung cancer. Opt Express 2010; 18: pp. 16.
6. Shankar L.K., Van den Abbeele A., Yap J., et. al.: Considerations for the use of imaging tools for phase II treatment trials in oncology. Clin Cancer Res 2009; 15: pp. 1891-1897.
7. Zhao B., Schwartz L.H., Larson S.M.: Imaging surrogates of tumor response to therapy: anatomic and functional biomarkers. J Nucl Med 2009; 50: pp. 239-249.
8. Maitland M.L.: Volumes to learn: advancing therapeutics with innovative computed tomography image data analysis. Clin Cancer Res 2010; 16: pp. 4493-4495.
9. Nishino M., Jackman D.M., Hatabu H., et. al.: Imaging of lung cancer in the era of molecular medicine. Acad Radiol 2011; 18: pp. 424-436.
10. Koshariya M., Jagad R.B., Kawamoto J., et. al.: An update and our experience with metastatic liver disease. Hepatogastroenterology 2007; 54: pp. 2232-2239.
11. Jaffe C.C.: Measures of response: RECIST, WHO, and new alternatives. J Clin Oncol 2006; 24: pp. 3245-3251.
12. Gavrielides M.A., Kinnard L.M., Myers K.J., et. al.: Noncalcified lung nodules: volumetric assessment with thoracic CT. Radiology 2009; 251: pp. 26-37.
13. Petrick N., Kim H.J.G., Clunie D., et. al.: Comparison of 1D, 2D, and 3D nodule sizing methods by radiologists for spherical and complex nodules on thoracic CT phantom images. Acad Radiol 2014; 21: pp. 30-40.
14. Zhao B., Lee S., Lee H.J., et. al.: Inter-reader and intra-reader variability in assessing change of total tumor volume.CARS—computer assisted radiology and surgery.2014. Fukuoka, Japan
15. Fenimore C., Lu Z., McNitt-Gray M.F., et. al.: Clinician sizing of synthetic nodules to evaluate CT interscanner effects.RSNA.2012.McCoromick PlaceChicago, IL:
16. Lal B.K., Beach K.W., Roubin G.S., et. al.: Restenosis after carotid artery stenting and endarterectomy: a secondary analysis of CREST, a randomised controlled trial. Lancet Neurol 2012; 11: pp. 755-763.
17. Mozley P.D., Bendtsen C., Zhao B., et. al.: Measurement of tumor volumes improves RECIST-based response assessments in advanced lung cancer. Transl Oncol 2012; 5: pp. 19-25.
18. McNitt-Gray M.F., Kim H., Zhao B., et. al.: Estimating the minimum detectable change of lung lesions using patient datasets acquired under a “no change” condition.RSNA.2011.McCormick PlaceChicago, IL:
19. Naidich D.P., Bankier A.A., MacMahon H., et. al.: Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 2013; 266: pp. 304-317.
20. Sieren J., Smith A., Thiesse J., et. al.: Exploration of the volumetric composition of human lung cancer nodules in correlated histopathology and computed tomography. Lung Cancer 2011; 74: pp. 61-68.
21. Chang B., Hwang J.H., Choi Y.-H., et. al.: Natural history of pure ground-glass opacity lung nodules detected by low-dose CT scan. Chest 2013; 143: pp. 172-178.
22. Kawata Y., Niki N., Ohmatsu H., et. al.: Quantitative classification based on CT histogram analysis of non-small cell lung cancer: correlation with histopathological characteristics and recurrence-free survival. Med Phys 2012; 39: pp. 988-1000.
23. Koo C.W., Miller W.T., Kucharczuk J.C.: Focal ground-glass opacities in non-small cell lung carcinoma resection patients. Eur J Radiol 2012; 81: pp. 139-145.
24. Zhang Y., Qiang J.W., Ye J.D., et. al.: High resolution CT in differentiating minimally invasive component in early lung adenocarcinoma. Lung Cancer 2014; 84: pp. 236-241.
25. Lee H.J., Goo J.M., Lee C.H., et. al.: Predictive CT findings of malignancy in ground-glass nodules on thin-section chest CT: the effects on radiologist performance. Eur Radiol 2009; 19: pp. 552-560.
26. Gandara D.R., Aberle D., Lau D., et. al.: Radiographic imaging of bronchioloalveolar carcinoma: screening, patterns of presentation and response assessment. J Thorac Oncol 2006; 1: pp. S20-S26.
27. Nagao M., Murase K., Yasuhara Y., et. al.: Measurement of localized ground-glass attenuation on thin-section computed tomography images: correlation with the progression of bronchioloalveolar carcinoma of the lung. Invest Radiol 2002; 37: pp. 692-697.
28. Sone S., Sakai F., Takashima S., et. al.: Factors affecting the radiologic appearance of peripheral bronchogenic carcinomas. J Thorac Imaging 1997; 12: pp. 159-172.
29. Gardiner N., Jogai S., Wallis A.: The revised lung adenocarcinoma classification—an imaging guide. J Thorac Dis 2014; 6: pp. S537-S546.
30. Mulshine J.L., Henschke C.I.: Lung cancer screening: achieving more by intervening less. Lancet Oncol 2014; 15: pp. 1284-1285.
31. Xu D.M., van Klaveren R.J., de Bock G.H., et. al.: Limited value of shape, margin and CT density in the discrimination between benign and malignant screen detected solid pulmonary nodules of the NELSON trial. Eur J Radiol 2008; 68: pp. 347-352.
32. Oda S., Awai K., Liu D., et. al.: Ground-glass opacities on thin-section helical CT: differentiation between bronchioloalveolar carcinoma and atypical adenomatous hyperplasia. AJR Am J Roentgenol 2008; 190: pp. 1363-1368.
33. Wagnetz U., Menezes R.J., Boerner S., et. al.: CT screening for lung cancer: implication of lung biopsy recommendations. AJR Am J Roentgenol 2012; 198: pp. 351-358.
34. Park C.M., Goo J.M., Kim T.J., et. al.: Pulmonary nodular ground-glass opacities in patients with extrapulmonary cancers: what is their clinical significance and how can we determine whether they are malignant or benign lesions?. Chest 2008; 133: pp. 1402-1409.
35. Lee S.M., Park C.M., Goo J.M., et. al.: Transient part-solid nodules detected at screening thin-section CT for lung cancer: comparisonwith persistent part-solid nodules 1. Radiology 2010; 255: pp. 242-251.
36. Alic L., Niessen W.J., Veenland J.F.: Quantification of heterogeneity as a biomarker in tumor imaging: a systematic review. PLoS ONE 2014; 9: pp. e110300.
37. Khan A.N., Al-Jahdali H.H., Allen C.M., et. al.: The calcified lung nodule: what does it mean?. Ann Thorac Med 2010; 5: pp. 67-79.
38. Kim T.J., Goo J.M., Lee K.W., et. al.: Clinical, pathological and thin-section CT features of persistent multiple ground-glass opacity nodules: comparison with solitary ground-glass opacity nodule. Lung Cancer 2009; 64: pp. 171-178.
39. Zhang L., Yankelevitz D.F., Carter D., et. al.: Internal growth of nonsolid lung nodules: radiologic-pathologic correlation. Radiology 2012; 263: pp. 279-286.
40. Goldstraw P.: The 7th edition of TNM in lung cancer: what now?. J Thorac Oncol 2009; 4: pp. 671-673.
41. Maldonado F., Boland J.M., Raghunath S., et. al.: Non-invasive characterization of the histopathologic features of pulmonary nodules of the lung adenocarcinoma spectrum using Computer Aided Nodule Assessment and Risk Yield (CANARY)—a pilot study. J Thorac Oncol 2013; 8: pp. 452.
42. Bhure U., Lardinois D., Kalff V., et. al.: Accuracy of CT parameters for assessment of tumour size and aggressiveness in lung adenocarcinoma with bronchoalveolar elements.2014.
43. Travis W.D., Brambilla E., Noguchi M., et. al.: International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society: international multidisciplinary classification of lung adenocarcinoma: executive summary. Proc Am Thorac Soc 2011; 8: pp. 381-385.
44. Warth A., Muley T., Meister M., et. al.: The novel histologic International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification system of lung adenocarcinoma is a stage-independent predictor of survival. J Clin Oncol 2012; 30: pp. 1438-1446.
45. Cronin P., Dwamena B.A., Kelly A.M., et. al.: Solitary pulmonary nodules: meta-analytic comparison of cross-sectional imaging modalities for diagnosis of malignancy 1. Radiology 2008; 246: pp. 772-782.
46. Agrawal S., Raj M.K., Kheruka S.C., et. al.: Utility of single photon emission computed tomography perfusion scans in radiation treatment planning of locally advanced lung cancers. Indian J Nucl Med 2012; 27: pp. 10-15.
47. Carvalho S., Leijenaar R.T.H., Velazquez E.R., et. al.: Prognostic value of metabolic metrics extracted from baseline positron emission tomography images in non-small cell lung cancer. Acta Oncol (Madr) 2013; 52: pp. 1398-1404.
48. de Figueiredo B., Antoine M., Trouette R., et. al.: Use of FDG-PET to guide dose prescription heterogeneity in stereotactic body radiation therapy for lung cancers with volumetric modulated arc therapy: a feasibility study. Radiat Oncol 2014; 9: pp. 300.
49. Mahasittiwat P., Yuan S., Xie C., et. al.: Metabolic tumor volume on PET reduced more than gross tumor volume on CT during radiotherapy in patients with non-small cell lung cancer treated with 3DCRT or SBRT. J Radiat Oncol 2013; 2: pp. 191-202.
50. Nair V.S., Keu K.V., Luttgen M.S., et. al.: An observational study of circulating tumor cells and (18)F-FDG PET uptake in patients with treatment-naive non-small cell lung cancer. PLoS ONE 2013; 8: pp. e67733.
51. Nestle U., Kremp S., Schaefer-Schuler A., et. al.: Comparison of different methods for delineation of 18F-FDG PET—positive tissue for target volume definition in radiotherapy of patients with non–small cell lung cancer. J Nucl Med 2005; 46: pp. 1342-1348.
52. Ohno T., Oshiro Y., Mizumoto M., et. al.: Comparison of dose–volume histograms between proton beam and X-ray conformal radiotherapy for locally advanced non-small-cell lung cancer. J Radiat Res (Tokyo) 2015; 56: pp. 128-133.
53. Sauter A.W., Winterstein S., Spira D., et. al.: Multifunctional profiling of non–small cell lung cancer using 18F-FDG PET/CT and volume perfusion CT. J Nucl Med 2012; 53: pp. 521-529.
54. Wang Y.-C., Tseng H.-L., Lin Y.-H., et. al.: Improvement of internal tumor volumes of non-small cell lung cancer patients for radiation treatment planning using interpolated average CT in PET/CT. PLoS ONE 2013; 8: pp. e64665.
55. Xue J., Zheng J., Guo H., et. al.: Predictive value of 18F-fluorodeoxyglucose positron emission tomography-computed tomography compared to postoperative pathological findings for patients with non-small cell lung cancer. Mol Clin Oncol 2015; 3: pp. 109-114.
56. Kauczor H.-U., Ley-Zaporozhan J., Ley S.: Imaging of pulmonary pathologies: focus on magnetic resonance imaging. Proc Am Thorac Soc 2009; 6: pp. 458-463.
57. Prosch H., Schaefer-Prokop C.: Screening for lung cancer. Curr Opin Oncol 2014; 26: pp. 131-137.
58. Manser R., Lethaby A., Irving L.B., et. al.: Screening for lung cancer. Cochrane Database Syst Rev 2013; CD001991
59. Gould M.K., Donington J., Lynch W.R., et. al.: Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013; 143: pp. e93S-e120S.
60. Bach P.B., Mirkin J.N., Oliver T.K., et. al.: Benefits and harms of CT screening for lung cancer: a systematic review. JAMA 2012; 307: pp. 2418-2429.
61. Pyenson B.S., Sander M.S., Jiang Y., et. al.: An actuarial analysis shows that offering lung cancer screening as an insurance benefit would save lives at relatively low cost. Health Aff (Millwood) 2012; 31: pp. 770-779.
62. Sox H.C.: Better evidence about screening for lung cancer. N Engl J Med 2011; 365: pp. 455-457.
63. Baldwin D., Duffy S., Wald N., et. al.: UK Lung Screen (UKLS) nodule management protocol: modelling of a single screen randomised controlled trial of low-dose CT screening for lung cancer. Thorax 2011; 66: pp. 308-313.
64. Jett J.R.: Limitations of screening for lung cancer with low-dose spiral computed tomography. Clin Cancer Res 2005; 11: pp. 4988s-4992s.
65. Wardwell N.R., Massion P.P.: Novel strategies for the early detection and prevention of lung cancer. Semin Oncol 2005; 32: pp. 259-268.
66. Swensen S.J., Jett J.R., Hartman T.E., et. al.: Lung cancer screening with CT: Mayo Clinic experience 1. Radiology 2003; 226: pp. 756-761.
67. Wender R., Fontham E.T.H., Barrera E., et. al.: American Cancer Society lung cancer screening guidelines. CA Cancer J Clin 2013; 63: pp. 107-117.
68. Xie X., Heuvelmans M.A., van Ooijen P.M.A., et. al.: A practical approach to radiological evaluation of CT lung cancer screening examinations. Cancer Imaging 2013; 13: pp. 391-399.
69. Wood D.E., Eapen G.A., Ettinger D.S., et. al.: Lung cancer screening. J Natl Compr Canc Netw 2012; 10: pp. 240-265.
70. Jaklitsch M.T., Jacobson F.L., Austin J.H., et. al.: The American Association for Thoracic Surgery guidelines for lung cancer screening using low-dose computed tomography scans for lung cancer survivors and other high-risk groups. J Thorac Cardiovasc Surg 2012; 144: pp. 33-38.
71. Takashima S., Sone S., Li F., et. al.: Small solitary pulmonary nodules (≤1 cm) detected at population-based CT Screening for lung cancer: reliable high-resolution CT features of benign lesions. AJR Am J Roentgenol 2003; 180: pp. 955-964.
72. Henschke C.I., Yankelevitz D.F.: CT screening for lung cancer: update 2007. Oncologist 2008; 13: pp. 65-78.
73. Henschke C.I., Yankelevitz D.F., Libby D.M., et. al.: Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med 2006; 355: pp. 1763-1771.
74. International Early Lung and Cardiac Action Program : I-ELCAP. Available at: http://www.ielcap.org/ Cited March 13, 2015
75. Horeweg N., Van Der Aalst C.M., Thunnissen E., et. al.: Characteristics of lung cancers detected by computer tomography screening in the randomized NELSON trial. Am J Respir Crit Care Med 2013; 187: pp. 848-854.
76. van Klaveren R.J., Oudkerk M., Prokop M., et. al.: Management of lung nodules detected by volume CT scanning. N Engl J Med 2009; 361: pp. 2221-2229.
77. Wang Y., van Klaveren R.J., van der Zaag-Loonen H.J., et. al.: Effect of nodule characteristics on variability of semiautomated volume measurements in pulmonary nodules detected in a lung cancer screening program. Radiology 2008; 248: pp. 625-631.
78. Aberle D.R., Adams A.M., Berg C.D., et. al.: Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365: pp. 395-409.
79. National Cancer Institute : National lung cancer screening trial. September 8; Available at: http://www.cancer.gov/clinicaltrials/noteworthy-trials/nlst Cited March 13, 2015
80. Matsuguma H., Mori K., Nakahara R., et. al.: Characteristics of subsolid pulmonary nodules showing growth during follow-up with CT scanning. Chest 2013; 143: pp. 436-443.
81. Mulshine J.L., D’Amico A.: Issues with implementing a high-quality lung cancer screening program. CA Cancer J Clin 2014; 64: pp. 352-363.
82. Moyer V.A.: Screening for lung cancer: U.S. preventive services task force recommendation statement. Ann Intern Med 2014; 160: pp. 330-338.
83. Medicare C.F., Services M.: Proposed decision memo for screening for lung cancer with low dose computed tomography (LDCT) (CAG-00439N).2014.
84. American Society of Clinical Oncology : The role of CT for lung cancer in clinical practice. The evidence based proactive guideline of the American College of Chest Physicians and the American Society for Clinical Oncology. Available at: http://www.asco.org/quality-guidelines/role-ct-screening-lung-cancer-clinical-practice-evidence-based-practice-guideline Cited November 25, 2014
85. National Guideline Clearinghouse : American Cancer Society lung cancer screening guidelines. Available at: http://www.guideline.gov/content.aspx?id=43894 Cited November 25, 2014
86. Henschke C.I., Yip R., Yankelevitz D.F., et. al.: Definition of a positive test result in computed tomography screening for lung cancer—a cohort study. Ann Intern Med 2013; 158: pp. 246-252.
87. Kazerooni E.A., Austin J.H.M., Black W.C., et. al.: ACR–STR practice parameter for the performance and reporting of lung cancer screening thoracic computed tomography (CT): 2014 (Resolution 4). J Thorac Imaging 2014; 29: pp. 310-316.
88. Gierada D.S., Pinsky P., Nath H., et. al.: Projected outcomes using different nodule sizes to define a positive CT lung cancer screening examination. J Natl Cancer Inst 2014; 106: pp. dju284.
89. American College of Radiology : Lung CT screening reporting and data system (lung-RADS). Available at: http://www.acr.org/Quality-Safety/Resources/LungRADS Cited November 25, 2014
90. Goldstraw P., Crowley J., Chansky K., et. al.: The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of Malignant Tumours. J Thorac Oncol 2007; 2: pp. 706-714.
91. Sargent D.J., Rubinstein L., Schwartz L., et. al.: Validation of novel imaging methodologies for use as cancer clinical trial end-points. Eur J Cancer 2009; 45: pp. 290-299.
92. Wakelee H., Chhatwani L.: Adjuvant chemotherapy for resected non-small cell lung cancer. Semin Thorac Cardiovasc Surg 2008; 20: pp. 198-203.
93. Mulshine J.L.: Early lung cancer detection: approaching the ‘tipping point’?. Oncology 2006; 20: pp. 1632.
94. Takiguchi Y., Sekine I., Iwasawa S.: Overdiagnosis in lung cancer screening with low-dose computed tomography. J Thorac Oncol 2013; 8: pp. e101-e102.
95. Humphrey L., Deffebach M., Pappas M., et. al.: Screening for lung cancer: systematic review to update the US Preventive Services Task Force recommendation.2013.
96. Lee H.Y., Lee K.S.: Ground-glass opacity nodules: histopathology, imaging evaluation, and clinical implications. J Thorac Imaging 2011; 26: pp. 106-118.
97. Kadota K., Villena-Vargas J., Yoshizawa A., et. al.: Prognostic significance of adenocarcinoma in situ, minimally invasive adenocarcinoma, and nonmucinous lepidic predominant invasive adenocarcinoma of the lung in patients with stage I disease. Am J Surg Pathol 2014; 38: pp. 448-460.
98. Henschke C.I., Yankelevitz D.F., Yip R., et. al.: Lung cancers diagnosed at annual CT screening: volume doubling times. Radiology 2012; 263: pp. 578-583.
99. Stember J.N., Ko J.P., Naidich D.P., et. al.: The self-overlap method for assessment of lung nodule morphology in chest CT. J Digit Imaging 2013; 26: pp. 239-247.
100. El-Baz A., Beache G.M., Gimel’farb G., et. al.: Computer-aided diagnosis systems for lung cancer: challenges and methodologies. Int J Biomed Imaging 2013; 2013:
101. Wiemker R., Rogalla P., Blaffert T., et. al.: Aspects of computer-aided detection (CAD) and volumetry of pulmonary nodules using multislice CT. Br J Radiol 2005; 78: pp. S46.
102. Abe Y., Hanai K., Nakano M., et. al.: A computer-aided diagnosis (CAD) system in lung cancer screening with computed tomography. Anticancer Res 2005; 25: pp. 483-488.
103. Petrick N., Kim H.J.G., Clunie D., et. al.: Evaluation of 1D, 2D and 3D nodule size estimation by radiologists for spherical and non-spherical nodules through CT thoracic phantom imaging. Proc SPIE 2011; 7963: pp. 79630D.
104. Kinnard L.M., Gavrielides M.A., Myers K.J., et. al.: Volume error analysis for lung nodules attached to pulmonary vessels in an anthropomorphic thoracic phantom. Proc SPIE 2008; 6915: pp. 69152Q.
105. Gavrielides M.A., Zeng R., Kinnard L.M., et. al.: A template-based approach for the analysis of lung nodules in a volumetric CT phantom study. Proc SPIE 2009; 7260: pp. 726009.
106. Winer-Muram H.T., Jennings S.G., Meyer C.A., et. al.: Effect of varying CT section width on volumetric measurement of lung tumors and application of compensatory equations. Radiology 2003; 229: pp. 184-194.
107. Ravenel J.G., Leue W.M., Nietert P.J., et. al.: Pulmonary nodule volume: effects of reconstruction parameters on automated measurements—a phantom study. Radiology 2008; 247: pp. 400-408.
108. Borradaile K., Ford R.: Discordance between BICR readers. Appl Clin Trials 2010; Nov 1
109. Gavrielides M.A., Zeng R., Myers K.J., et. al.: Benefit of overlapping reconstruction for improving the quantitative assessment of CT lung nodule volume. Acad Radiol 2012; 20: pp. 173-180.
110. Gavrielides M.A., Zeng R., Kinnard L.M., et. al.: Information-theoretic approach for analyzing bias and variance in lung nodule size estimation with CT: a phantom study. IEEE Trans Med Imaging 2010; 29: pp. 1795-1807.
111. Gavrielides M.A., Kinnard L.M., Myers K.J., et. al.: A resource for the assessment of lung nodule size estimation methods: database of thoracic CT scans of an anthropomorphic phantom. Opt Express 2010; 18: pp. 15244-15255.
112. Das M., Ley-Zaporozhan J., Gietema H.A., et. al.: Accuracy of automated volumetry of pulmonary nodules across different multislice CT scanners. Eur Radiol 2007; 17: pp. 1979-1984.
113. Bolte H., Riedel C., Muller-Hulsbeck S., et. al.: Precision of computer-aided volumetry of artificial small solid pulmonary nodules in ex vivo porcine lungs. Br J Radiol 2007; 80: pp. 414-421.
114. Cagnon C.H., Cody D.D., McNitt-Gray M.F., et. al.: Description and implementation of a quality control program in an imaging-based clinical trial. Acad Radiol 2006; 13: pp. 1431-1441.
115. Goodsitt M.M., Chan H.P., Way T.W., et. al.: Accuracy of the CT numbers of simulated lung nodules imaged with multi-detector CT scanners. Med Phys 2006; 33: pp. 3006-3017.
116. Oda S., Awai K., Murao K., et. al.: Computer-aided volumetry of pulmonary nodules exhibiting ground-glass opacity at MDCT. AJR Am J Roentgenol 2010; 194: pp. 398-406.
117. McNitt-Gray M.F., Bidaut L.M., Armato S.G., et. al.: Computed tomography assessment of response to therapy: tumor volume change measurement, truth data, and error. Transl Oncol 2009; 2: pp. 216-222.
118. Keil S., Plumhans C., Behrendt F.F., et. al.: Semi-automated quantification of hepatic lesions in a phantom. Invest Radiol 2009; 44: pp. 82-88.
119. Brandman S., Ko J.P.: Pulmonary nodule detection, characterization, and management with multidetector computed tomography. J Thorac Imaging 2011; 26: pp. 90-105.
120. Park C.M., Goo J.M., Lee H.J., et. al.: Nodular ground-glass opacity at thin-section CT: histologic correlation and evaluation of change at follow-up 1. Radiographics 2007; 27: pp. 391-408.
121. Awai K., Murao K., Ozawa A., et. al.: Pulmonary nodules: estimation of malignancy at thin-section helical CT—effect of computer-aided diagnosis on performance of radiologists 1. Radiology 2006; 239: pp. 276-284.
122. Sakurai H., Maeshima A., Watanabe S., et. al.: Grade of stromal invasion in small adenocarcinoma of the lung: histopathological minimal invasion and prognosis. Am J Surg Pathol 2004; 28: pp. 198-206.
123. Tan B.B., Flaherty K.R., Kazerooni E.A., et. al.: The solitary pulmonary nodule. Chest 2003; 123: pp. 89S-96S.
124. Swensen S.J.: Functional CT: lung nodule evaluation 1. Radiographics 2000; 20: pp. 1178-1181.
125. Radiological Society of North America : Quantitative Imaging Biomarkers Alliance. Available at: https://www.rsna.org/qiba/ Cited March 13, 2015