Rationale and Objectives
The aims of this study were to investigate the association between 8-week tumor volume decrease and survival in an independent cohort of epidermal growth factor receptor ( EGFR )-mutant advanced non-small cell lung cancer (NSCLC) patients treated with first-line erlotinib or gefitinib, and to assess the rate of their volumetric tumor growth after the volume nadir.
Materials and Methods
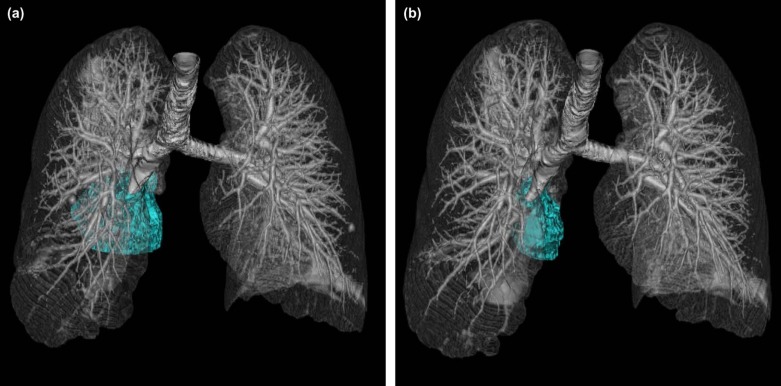
In patients with advanced NSCLC harboring sensitizing EGFR mutations treated with first-line erlotinib or gefitinib, computed tomography (CT) tumor volumes of dominant lung lesions were analyzed for (1) the association with survival, and (2) the volumetric tumor growth rate after the volume nadir.
Results
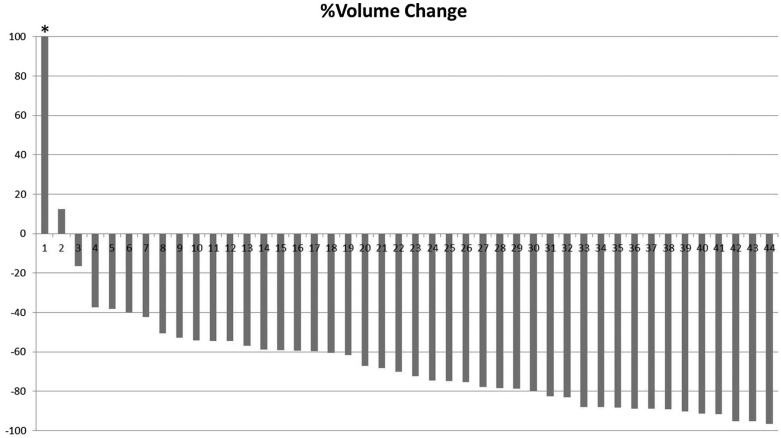
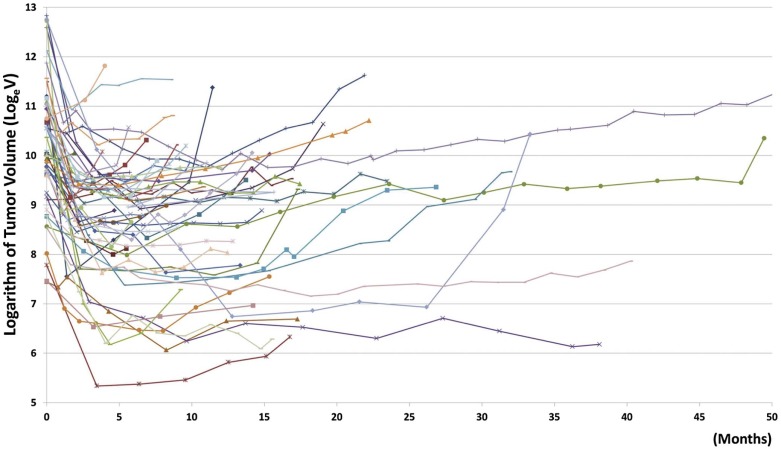
In 44 patients with the 8-week follow-up CT, the 8-week tumor volume decrease (%) was significantly associated with longer overall survival when fitted as a continuous variable in a Cox model ( P = 0.01). The growth rate of the logarithm of tumor volume (log e V), obtained using a linear mixed-effects model adjusting for time since baseline, was 0.096/month (SE: 0.013/month; 95% confidence interval [CI]: 0.071–0.12/month), which was similar to the rate of 0.12/month (SE: 0.015/month; 95%CI: 0.090–0.15/month) observed in the previous report.
Conclusions
The 8-week tumor volume decrease was validated as a marker for longer survival in the independent cohort of EGFR -mutant NSCLC patients treated with first-line erlotinib or gefitinib. The volumetric tumor growth rate after the nadir in this cohort was similar to that of the previous cohort, indicating the reproducibility of the observation among different patient cohorts.
Introduction
The discoveries of genomic abnormalities in the tumors from patients with lung cancer and the effective treatment with targeted agents have ushered in a new era of therapeutic approaches to lung cancer . Epidermal growth factor receptor ( EGFR ) mutations in non-small cell lung cancer (NSCLC) have been studied as one of the major therapeutic targets since their discovery in 2004 . Patients with NSCLC harboring sensitizing EGFR mutations have initial dramatic responses to the EGFR tyrosine kinase inhibitors (TKIs), erlotinib, gefitinib, and afatinib, with response rates of 55–83% and progression-free survival (PFS) of 9.7–13.1 months . However, their tumors eventually grow back during EGFR -TKI therapy due to the development of acquired resistance, eventually leading to tumor progression . The duration of disease control from EGFR -TKI therapy can range from 4 months to 4 years or longer . In this context, objective early markers of tumor response during EGFR -TKI therapy are needed to identify patients who can safely remain on therapy and those who are unlikely to have long-term control and may potentially benefit from an early introduction of additional or alternative agents.
Imaging remains as the principal method to objectively characterize the tumor burden during cancer therapy . Prior studies have demonstrated the limitations of the conventional diameter-based approach according to Response Evaluation Criteria in Solid Tumors (RECIST) and indicated the need for volumetric tumor assessment . The previous studies evaluated tumor volume measurements in patients with advanced NSCLC treated with EGFR -TKIs using Food and Drug Administration-approved, commercially available software and published the high reproducibility of the technique . By applying this technique to patients with EGFR -mutant NSCLC treated with the first-line erlotinib or gefitinib, the study demonstrated that greater tumor volume decrease at 8 weeks of therapy is significantly associated with longer overall survival (OS), with a cut-off value of 38% volume decrease at 8 weeks best differentiating patients with longer OS and PFS . The 8-week volume change as a predictor of survival has a potential role in identifying patients who may benefit from additional or alternative therapy in the early course of therapy, and help in maximizing the benefit of targeted therapy and in improving the clinical outcome. Tumor volume analysis was also applied to characterize the rate of tumor growth in patients with EGFR -mutant NSCLC after they reach their volume nadir (the smallest tumor volume since baseline), which is another important aspect in assessing benefit of cancer therapy . A prior study reported a reference value of the volumetric tumor growth rate among these patients after their volume nadir, which helps to differentiate slow versus fast progressors among those who are on EGFR -TKI therapy, thus contributing to provide an objective guidance about when to keep patients on the EGFR -TKI after progression .
Get Radiology Tree app to read full this article<
Materials and Methods
Patients
Get Radiology Tree app to read full this article<
CT Tumor Volume Measurements during TKI Therapy
Get Radiology Tree app to read full this article<
The 8-week Tumor Volume Analysis
Get Radiology Tree app to read full this article<
Volumetric Tumor Growth after the Nadir
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
The 8-week Tumor Volume Decrease and Survival
Get Radiology Tree app to read full this article<
Table 1
Demographics and Disease Characteristics of 44 Patients with 8-week Scan
Variables Category Age Median (range) 66.5 years (26–88) Sex Female 30 Male 14 Race White 37 Black 3 Asian 2 Other 2 Smoking status Never 42 Former 1 Current 1 Pathology Adenocarcinoma 43 Unknown 1 ECOG PS 0 18 1 16 2 5 3 1 Unknown 4 Extrathoracic metastasis Present 26 Absent 18EGFR -TKI Erlotinib 33 Gefitinib 11EGFR mutations Exon19 del 22 L858R 20 L861Q 1 G719 1
ECOG, Eastern Cooperative Oncology Group; EGFR , epidermal growth factor receptor; PS, performance status; TKI, tyrosine kinase inhibitor.
The values represent the number of patients unless otherwise specified.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Volumetric Tumor Growth after the Nadir
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
logeV=0.093×time+0.62×logeV0+0.39×stage+0.39×TKI−0.11×smoking+0.10 log
e
V
=
0.093
×
time
+
0.62
×
log
e
V
0
+
0.39
×
stage
+
0.39
×
TKI
−
0.11
×
smoking
+
0.10
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conflicts of Interest
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Acknowledgements
Get Radiology Tree app to read full this article<
References
1. Kris M.G., Johnson B.E., Berry L.D., et. al.: Using multiplexed assays of oncogenic drivers in lung cancers to select targeted drugs. JAMA 2014; 311: pp. 1998-2006.
2. Nishino M., Hatabu H., Johnson B.E., et. al.: State of the art: response assessment in lung cancer in the era of genomic medicine. Radiology 2014; 271: pp. 6-27.
3. Lynch T.J., Bell D.W., Sordella R., et. al.: Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 2004; 350: pp. 2129-2139.
4. Paez J.G., Janne P.A., Lee J.C., et. al.: EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 2004; 304: pp. 1497-1500.
5. Pao W., Miller V., Zakowski M., et. al.: EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A 2004; 101: pp. 13306-13311.
6. Zhou C., Wu Y.L., Chen G., et. al.: Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 2011; 12: pp. 735-742.
7. Yang K., Kim .D., Planchard D., et. al.: Updated safety and efficacy from a phase I study of AZD9291 in patients (pts) with EGFR-TKI-resistant non-small cell lung cancer (NSCLC). ESMO2014.
8. Sequist L.V., Martins R.G., Spigel D., et. al.: First-line gefitinib in patients with advanced non-small-cell lung cancer harboring somatic EGFR mutations. J Clin Oncol 2008; 26: pp. 2442-2449.
9. Mok T.S., Wu Y.L., Thongprasert S., et. al.: Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009; 361: pp. 947-957.
10. Maemondo M., Inoue A., Kobayashi K., et. al.: Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010; 362: pp. 2380-2388.
11. Jackman D.M., Yeap B.Y., Sequist L.V., et. al.: Exon 19 deletion mutations of epidermal growth factor receptor are associated with prolonged survival in non-small cell lung cancer patients treated with gefitinib or erlotinib. Clin Cancer Res 2006; 12: pp. 3908-3914.
12. Rosell R., Carcereny E., Gervais R., et. al.: Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012; 13: pp. 239-246.
13. Sequist L.V., Waltman B.A., Dias-Santagata D., et. al.: Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 2011; 3: pp. 75ra26.
14. Nishino M., Guo M., Jackman D.M., et. al.: CT tumor volume measurement in advanced non-small-cell lung cancer: performance characteristics of an emerging clinical tool. Acad Radiol 2011; 18: pp. 54-62.
15. Nishino M., Jagannathan J.P., Krajewski K.M., et. al.: Personalized tumor response assessment in the era of molecular medicine: cancer-specific and therapy-specific response criteria to complement pitfalls of RECIST. AJR Am J Roentgenol 2012; 198: pp. 737-745.
16. Erasmus J.J., Gladish G.W., Broemeling L., et. al.: Interobserver and intraobserver variability in measurement of non-small-cell carcinoma lung lesions: implications for assessment of tumor response. J Clin Oncol 2003; 21: pp. 2574-2582.
17. Mozley P.D., Bendtsen C., Zhao B., et. al.: Measurement of tumor volumes improves RECIST-based response assessments in advanced lung cancer. Transl Oncol 2012; 5: pp. 19-25.
18. Mozley P.D., Schwartz L.H., Bendtsen C., et. al.: Change in lung tumor volume as a biomarker of treatment response: a critical review of the evidence. Ann Oncol 2010; 21: pp. 1751-1755.
19. Zhao B., James L.P., Moskowitz C.S., et. al.: Evaluating variability in tumor measurements from same-day repeat CT scans of patients with non-small cell lung cancer. Radiology 2009; 252: pp. 263-272.
20. Zhao B., Schwartz L.H., Moskowitz C.S., et. al.: Lung cancer: computerized quantification of tumor response—initial results. Radiology 2006; 241: pp. 892-898.
21. Nishino M., Dahlberg S.E., Cardarella S., et. al.: Tumor volume decrease at 8 weeks is associated with longer survival in EGFR-mutant advanced non-small-cell lung cancer patients treated with EGFR TKI. J Thorac Oncol 2013; 8: pp. 1059-1068.
22. Looney W.B., Trefil J.S., Hopkins H.A., et. al.: Solid tumor models for assessment of different treatment modalities: therapeutic strategy for sequential chemotherapy with radiotherapy. Proc Natl Acad Sci U S A 1977; 74: pp. 1983-1987.
23. Demicheli R., Foroni R., Ingrosso A., et. al.: An exponential-Gompertzian description of LoVo cell tumor growth from in vivo and in vitro data. Cancer Res 1989; 49: pp. 6543-6546.
24. Gomez-Roca C., Koscielny S., Ribrag V., et. al.: Tumour growth rates and RECIST criteria in early drug development. Eur J Cancer 2011; 47: pp. 2512-2516.
25. Stein W.D., Gulley J.L., Schlom J., et. al.: Tumor regression and growth rates determined in five intramural NCI prostate cancer trials: the growth rate constant as an indicator of therapeutic efficacy. Clin Cancer Res 2011; 17: pp. 907-917.
26. Stein W.D., Wilkerson J., Kim S.T., et. al.: Analyzing the pivotal trial that compared sunitinib and IFN-alpha in renal cell carcinoma, using a method that assesses tumor regression and growth. Clin Cancer Res 2012; 18: pp. 2374-2381.
27. Ferte C., Fernandez M., Hollebecque A., et. al.: Tumor growth rate is an early indicator of antitumor drug activity in phase I clinical trials. Clin Cancer Res 2014; 20: pp. 246-252.
28. Nishino M., Dahlberg S.E., Cardarella S., et. al.: Volumetric tumor growth in advanced non-small cell lung cancer patients with EGFR mutations during EGFR-tyrosine kinase inhibitor therapy: developing criteria to continue therapy beyond RECIST progression. Cancer 2013; 119: pp. 3761-3768.
29. Nishino M., Cardarella S., Dahlberg S.E., et. al.: Radiographic assessment and therapeutic decisions at RECIST progression in EGFR-mutant NSCLC treated with EGFR tyrosine kinase inhibitors. Lung Cancer 2013; 79: pp. 283-288.
30. Nishino M., Cardarella S., Jackman D.M., et. al.: RECIST 1.1 in NSCLC patients with EGFR mutations treated with EGFR tyrosine kinase inhibitors: comparison with RECIST 1.0. AJR Am J Roentgenol 2013; 201: pp. W64-W71.
31. Nishino M., Jackman D.M., DiPiro P.J., et. al.: Revisiting the relationship between tumour volume and diameter in advanced NSCLC patients: an exercise to maximize the utility of each measure to assess response to therapy. Clin Radiol 2014; 69: pp. 841-848.
32. Gold K.A., Kim E.S., Lee J.J., et. al.: The BATTLE to personalize lung cancer prevention through reverse migration. Cancer Prev Res (Phila) 2011; 4: pp. 962-972.
33. Laird N.M., Ware J.H.: Random-effects models for longitudinal data. Biometrics 1982; 38: pp. 963-974.
34. McKeage K.: Alectinib: a review of its use in advanced ALK-rearranged non-small cell lung cancer. Drugs 2015; 75: pp. 75-82.
35. Sato T., Watanabe A., Kondo H., et. al.: Long-term results and predictors of survival after surgical resection of patients with lung cancer and interstitial lung diseases. J Thorac Cardiovasc Surg 2015; 149: pp. 64-69. 70.e1–2.
36. Kato M., Shukuya T., Takahashi F., et. al.: Pemetrexed for advanced non-small cell lung cancer patients with interstitial lung disease. BMC Cancer 2014; 14: pp. 508.
37. Camidge D.R., Bang Y.J., Kwak E.L., et. al.: Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol 2012; 13: pp. 1011-1019.
38. Kwak E.L., Bang Y.J., Camidge D.R., et. al.: Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med 2010; 363: pp. 1693-1703.
39. Shaw A.T., Kim D.W., Nakagawa K., et. al.: Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med 2013; 368: pp. 2385-2394.
40. Seto T., Kiura K., Nishio M., et. al.: CH5424802 (RO5424802) for patients with ALK-rearranged advanced non-small-cell lung cancer (AF-001JP study): a single-arm, open-label, phase 1-2 study. Lancet Oncol 2013; 14: pp. 590-598.
41. Park K., Ahn M.J., Yu C.J., et. al.: ASPIRATION: first-line erlotinib until and beyond RECIST progression in Asian patients with EGFR mutation-positive NSCLC. ESMO2014.
42. Soria J.C., Wu Y.L., Nakagawa K., et. al.: Gefitinib plus chemotherapy versus placebo plus chemotherapy in EGFR-mutation-positive non-small-cell lung cancer after progression on first-line gefitinib (IMPRESS): a phase 3 randomised trial. Lancet Oncol 2015; 16: pp. 990-998.
43. Kim H.S., Kim J.H.: Ideal number of target lesions per organ to measure in metastatic colorectal cancer. Oncol Lett 2014; 8: pp. 1896-1900.
44. Kim H.S., Kim J.H., Yang I.: Tumor response assessment by measuring the single largest lesion per organ in patients with advanced non-small cell lung cancer. Lung Cancer 2014; 85: pp. 385-389.
45. Kim H.S., Kim J.W., Kim J.H., et. al.: Single-lesion measurement per organ for assessing tumor response in advanced gastric cancer. Oncology 2014; 88: pp. 69-75.
46. Nishino M., Jagannathan J.P., Ramaiya N.H., et. al.: Revised RECIST guideline version 1.1: what oncologists want to know and what radiologists need to know. AJR Am J Roentgenol 2010; 195: pp. 281-289.