Rationale and Objectives
The increasing use of imaging in the emergency department (ED) services has become an important problem on the basis of cost and unnecessary exposure to radiation. Radiographic examination of the chest has been reported to be performed in 34.4% of ED visits, and chest computerized tomography (CCT) in 15.8%, whereas some patients receive both chest radiography and CCT in the same visit. In the current study, it was aimed to establish instances of medical waste and unnecessary radiation exposure and to show how the inclusion of radiologists in the ordering process would affect the amount of unnecessary imaging studies.
Materials and Methods
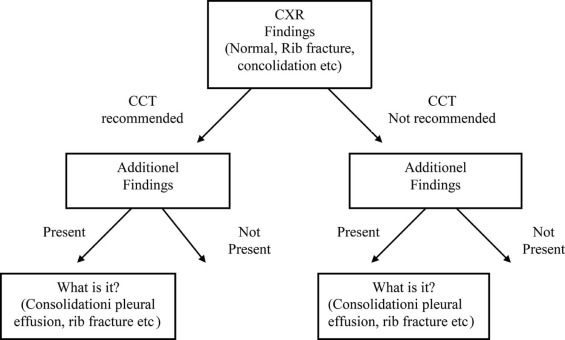
This retrospective study included 1012 ED patients who had both chest radiography and CCT during the same visit at Ankara Training and Research Hospital between April 2015 and January 2016. The patients were divided into subgroups of trauma and nontrauma. To detect unnecessary imaging examinations, data were analyzed according to the presence of additional findings on CCT images and the recommendation of a radiologist for CCT imaging.
Results
In the trauma group, 77.1% (461/598) and in the nontrauma group, 80.4% (334/414) of patients could be treated without any need for CCT. In the trauma group, the radiologist recommendation only, and in the nontrauma group, both the radiologist recommendation and the age were determined to be able to predict the risk of having additional findings on CCT.
Conclusions
Considering only the age of the patient before ordering CCT could decrease the rate of unnecessary imaging. Including radiologists into both the evaluation and the ordering processes may help to save resources and decrease exposure to ionizing radiation.
Introduction
From the beginning of the 20th century, imaging has been a rapidly growing field of physician services . Imaging studies are primarily performed in hospital outpatient facilities, private offices, hospital inpatient facilities, and emergency departments (ED) . The increasing use of imaging in ED services has attracted the attention of a significant number of researchers. Various studies have suggested that this increase, especially in cases of computerized tomography (CT), has higher costs but has not provided improved outcomes .
The number of ED visits has also increased from 123.8 million in 2008 to 136.3 million in 2011. It has been reported that radiographic examination of the chest is performed in 34.4% of ED visits, and a chest computerized tomography (CCT) in 15.8% of visits . Chest radiography (CXR) is applied at the ED visits of more than 70% of patients with acute cardiothoracic symptoms, CCT for the same indication in more than 13% of cases , and some patients receive both CXR and CCT in the same visit.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Materials and Methods
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Statistical Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Results
Patients
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 1
The Distribution of Additional Findings
Additional Findings Number (Percentage) Rib fracture 86(39.6) Consolidation 44(20.3) Contusion 36(16,6) Pleural effusion 36(16,6) Pulmonary embolism 25(11,5) Vertebral fracture 15(6,9) Pneumothorax/Hemothorax 14(6,5) Others(pericardial effusion, mediastinal emphysema, dissection, mass lesions, small airway disease, etc.) 5(2,3) Total 217(21,4)
Get Radiology Tree app to read full this article<
Trauma Versus Nontrauma
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Presence of Additional Findings
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Regression Analysis
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
TABLE 2
Regression Analysis Results
Variables Univariable Multivariable OR %95C.I.P OR %95C.I.P Lower Upper Lower Upper All population Age 1,160 1,090 1,230 <0,001 \* 1,150 1,070 1,230 <0,001 \* Radiologist recommendation (ref: not recommended) 4,752 3,334 6,774 <0,001 \* 4,145 2,282 7,529 <0,001 \* Sex (ref \\ :female) 1,381 0,996 1,915 0,053 — — — — CXR (ref:normal) 3,000 2,178 4,132 <0,001 \* — — — — Trauma (ref: nontraumatic) 1,241 0,910 1,691 0,172 — — — — Nagelkerke R 2 = 0,253; P < 0,001 \* Trauma group Radiologist recommendation (ref: not recommended) 3,791 2,268 6,336 <0,001 \* 3,772 1,711 8,316 0,001 \* Age 1,120 1,010 1,230 0,046 — — — — Sex (ref:female) 1,506 0,903 2,512 0,117 — — — — CXR (ref:normal) 2,381 1,448 3,915 0,001 \* — — — — Nagelkerke R 2 = 0,197; P < 0,001 \* Nontrauma group Age 1,240 1,140 1,340 <0,001 \* 1,180 1,080 1,290 <0,001 \* Radiologist recommendation (ref: not recommended) 9,417 5,281 16,792 <0,001 \* 4,490 1,753 11,500 0,002 \* Sex (ref:female) 1,249 0,813 1,917 0,310 — — — — CXR (ref:normal) 6,348 3,859 10,443 <0,001 \* — — — — Nagelkerke R 2 = 0,285; P < 0,001 \*
CXR, chest radiography; OR, odds ratio; 95% C.I., 95% confidence interval.
Stepwise backward method was used in multivariable regression models.
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Discussion
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Get Radiology Tree app to read full this article<
Conclusion
Get Radiology Tree app to read full this article<
References
1. Iglehart J.K.: Health insurers and medical-imaging policy—a work in progress. N Engl J Med 2009; 360: pp. 1030-1037.
2. Rao V.M., Levin D.C., Parker L., et. al.: Trends in utilization rates of the various imaging modalities in emergency departments: nationwide Medicare data from 2000 to 2008. J Am Coll Radiol 2011; 8: pp. 706-709.
3. Lee J., Kirschner J., Pawa S., et. al.: Computed tomography use in the adult emergency department of an academic urban hospital from 2001 to 2007. Ann Emerg Med 2010; 56: pp. 591-596.
4. Korley F.K., Pham J.C., Kirsch T.D.: Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998–2007. JAMA 2010; 304: pp. 1465-1471.
5. Hanna T.N., Shuaib W., Kerchberger J.M., et. al.: Inefficient resource use for patients who receive both a chest radiograph and chest CT in a single emergency department visit. J Am Coll Radiol 2016; 13: pp. 21-27.
6. Larson D.B., Johnson L.W., Schnell B.M., et. al.: National trends in CT use in the emergency department: 1995–2007. Radiology 2011; 258: pp. 164-173.
7. Smith-Bindman R., Lipson J., Marcus R., et. al.: Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med 2009; 169: pp. 2078-2086.
8. Griffey R.T., Sodickson A.: Cumulative radiation exposure and cancer risk estimates in emergency department patients undergoing repeat or multiple CT. AJR Am J Roentgenol 2009; 192: pp. 887-892.
9. Artamonov O.M., Samarin S.N., Kirschner J.: Coincidence electron spectroscopy of W(100) in the threshold-energy region. Phys Rev B Condens Matter 1995; 51: pp. 2491-2500.
10. Levin D.C., Rao V.M., Parker L., et. al.: Continued growth in emergency department imaging is bucking the overall trends. J Am Coll Radiol 2014; 11: pp. 1044-1047.
11. Ringel J.S., Eibner C., Girosi F., et. al.: Modeling health care policy alternatives. Health Serv Res 2010; 45: pp. 1541-1558.
12. Kamat A.B., Midgley S., Kimbrell K.: Duplication of radiology imaging studies in the emergency department: what is the cost?. Emerg Med J 2015; 32: pp. 144-148.
13. Hillestad R., Bigelow J., Bower A., et. al.: Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff 2005; 24: pp. 1103-1117.
14. Smith-Bindman R., Miglioretti D.L., Johnson E., et. al.: Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA 2012; 307: pp. 2400-2409.
15. Brenner D.J., Hall E.J.: Computed tomography—an increasing source of radiation exposure. N Engl J Med 2007; 357: pp. 2277-2284.
16. Pearce M.S., Salotti J.A., Little M.P., et. al.: Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380: pp. 499-505.
17. Langdorf M.I., Medak A.J., Hendey G.W., et. al.: Prevalence and clinical import of thoracic injury identified by chest computed tomography but not chest radiography in blunt trauma: multicenter prospective cohort study. Ann Emerg Med 2015; 66: pp. 589-600.
18. Kaiser M., Whealon M., Barrios C., et. al.: The clinical significance of occult thoracic injury in blunt trauma patients. Am Surg 2010; 76: pp. 1063-1066.
19. Kaiser M.L., Whealon M.D., Barrios C., et. al.: Risk factors for traumatic injury findings on thoracic computed tomography among patients with blunt trauma having a normal chest radiograph. Arch Surg 2011; 146: pp. 459-463.
20. Exadaktylos A.K., Sclabas G., Schmid S.W., et. al.: Do we really need routine computed tomographic scanning in the primary evaluation of blunt chest trauma in patients with “normal” chest radiograph?. J Trauma 2001; 51: pp. 1173-1176.
21. Cardinale L., Volpicelli G., Lamorte A., et. al.: Revisiting signs, strengths and weaknesses of Standard Chest Radiography in patients of Acute Dyspnea in the Emergency Department. J Thorac Dis 2012; 4: pp. 398-407.
22. Gatt M.E., Spectre G., Paltiel O., et. al.: Chest radiographs in the emergency department: is the radiologist really necessary?. Postgrad Med J 2003; 79: pp. 214-217.